C Difficile Colitis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | Diagnosis | TREATMENT | REFERENCES

Overview
Clostridium difficile (klos-TRID-e-um dif-uh-SEEL), also known as Clostridioides difficile and often referred to as C. difficile or C. diff, is a bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon.
Illness from C. difficile most commonly affects older adults in hospitals or in long-term care facilities and typically occurs after use of antibiotic medications.
However, studies show increasing rates of C. difficile infection among people traditionally not considered to be at high risk, such as young and healthy individuals who haven't used antibiotics and who haven't been in a healthcare facility.
Each year in the United States, about a half million people get sick from C. difficile, and in recent years, C. difficile infections have become more frequent, severe and difficult to treat. Recurrent C. difficile infections also are on the rise.
Causes
C. difficile bacteria are found throughout the environment — in soil, air, water, human and animal feces, and food products, such as processed meats. A small number of healthy people naturally carry the bacteria in their large intestines and don't have ill effects from the infection.
Spores from C. difficile bacteria are passed in feces and spread to food, surfaces and objects when people who are infected don't wash their hands thoroughly. These spores can persist in a room for weeks or months. If you touch a surface contaminated with C. difficile spores, you may then unknowingly swallow the bacteria.
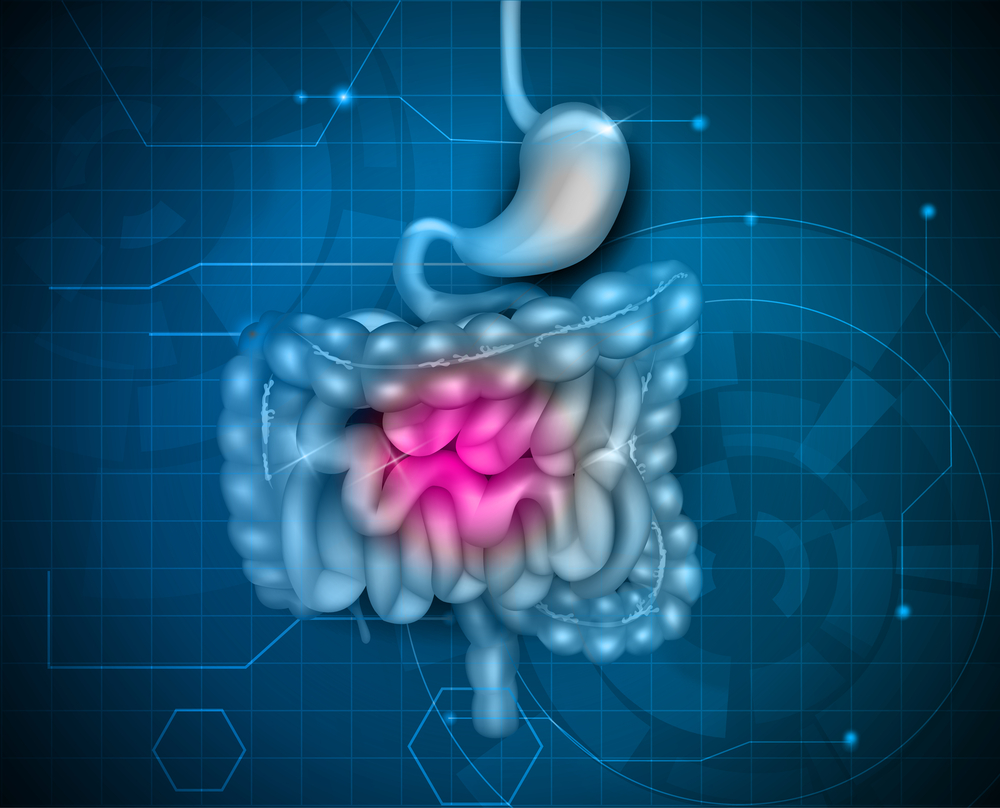
Once established, C. difficile can produce toxins that attack the lining of the intestine. The toxins destroy cells, produce patches (plaques) of inflammatory cells and decaying cellular debris inside the colon, and cause watery diarrhea.
Emergence of a new strain
An aggressive strain of C. difficile has emerged that produces far more toxins than other strains do. The new strain may be more resistant to certain medications and has shown up in people who haven't been in the hospital or taken antibiotics. This strain of C. difficile has caused several outbreaks of illness since 2000.
Risk factors
Although people who have no known risk factors have gotten sick from C. difficile, certain factors increase the risk.
1. Taking antibiotics or other medications
Your intestines contain about 100 trillion bacterial cells and up to 2,000 different kinds of bacteria, many of which help protect your body from infection. When you take an antibiotic to treat an infection, these drugs tend to destroy some of the normal, helpful bacteria in addition to the bacteria causing the infection. Without enough healthy bacteria to keep it in check, C. difficile can quickly grow out of control. The antibiotics that most often lead to C. difficile infections include:
- Fluoroquinolones
- Cephalosporins
- Penicillins
- Clindamycin
Proton pump inhibitors, a type of medicine used to reduce stomach acid, also may increase your risk of C. difficile infection.
2. Staying in a healthcare facility
The majority of C. difficile infections occur in people who are or who have recently been in a health care setting — including hospitals, nursing homes and long-term care facilities — where germs spread easily, antibiotic use is common and people are especially vulnerable to infection.
In hospitals and nursing homes, C. difficile spreads mainly on hands from person to person, but also on cart handles, bedrails, bedside tables, toilets, sinks, stethoscopes, thermometers — and even telephones and remote controls.
3. Having a serious illness or medical procedure
If you have a serious illness, such as inflammatory bowel disease or colorectal cancer, or a weakened immune system as a result of a medical condition or treatment (such as chemotherapy), you're more susceptible to a C. difficile infection. Your risk of C. difficile infection is also greater if you've had abdominal surgery or a gastrointestinal procedure.
4. Other risk factors
Women are more likely than men to have C. difficile infection.
Older age is a risk factor. In one study, the risk of becoming infected with C. difficile was 10 times greater for people age 65 and older compared with younger people.
Having one C. difficile infection increases your chance of having another one, and the risk continues to increase with each infection.
Symptoms
Some people carry the bacterium C. difficile in their intestines but never become sick, though rarely may still spread the infection.
Signs and symptoms usually develop within five to 10 days after starting a course of antibiotics, but may occur as soon as the first day or up to two months later.
1. Mild to Moderate Infection:
The most common signs and symptoms of mild to moderate C. difficile infection are:
-
Watery diarrhea three or more times a day for two or more days
-
Mild abdominal cramping and tenderness
2. Severe Infection:
People who have a severe C. difficile infection tend to become dehydrated and may need to be hospitalized.
C. difficile can cause the colon to become inflamed and sometimes form patches of raw tissue that can bleed or produce pus.
Signs and symptoms of severe infection include:
- Watery diarrhea 10 to 15 times a day
- Abdominal cramping and pain, which may be severe
- Rapid heart rate
- Fever
- Blood or pus in the stool
- Nausea
- Loss of appetite
- Weight loss
- Swollen abdomen
Severe C. difficile infection may also cause severe intestinal inflammation, enlargement of the colon (also called toxic megacolon) and sepsis. People who have these conditions are often admitted to the intensive care unit.
Complications
Complications of C. difficile infections include:
- Dehydration. Severe diarrhea can lead to a significant loss of fluids and electrolytes. This makes it difficult for your body to function normally and can cause blood pressure to drop to dangerously low levels.
- Kidney failure. In some cases, dehydration can occur so quickly that kidney function rapidly deteriorates (kidney failure).
- Toxic megacolon. In this rare condition, your colon is unable to expel gas and stool, causing it to become greatly distended (megacolon). Left untreated, your colon may rupture, causing bacteria from the colon to enter your abdominal cavity. An enlarged or ruptured colon requires emergency surgery and may be fatal.
- A hole in your large intestine (bowel perforation). This is rare and results from extensive damage to the lining of your large intestine or after toxic megacolon. A perforated bowel can spill bacteria from the intestine into your abdominal cavity, leading to a life-threatening infection (peritonitis).
- Death. Even mild to moderate C. difficile infections can quickly progress to fatal disease if not treated promptly.
Diagnosis
Doctors often suspect C. difficile in anyone who has diarrhea and who has other risk factors for C. difficile. In such cases, doctors are likely to order one or more of the following tests.
1. Stool tests
Toxins produced by C. difficile bacteria can usually be detected in a sample of your stool. Several main types of lab tests exist, and they include:
- Polymerase chain reaction. This sensitive molecular test can rapidly detect the C. difficile toxin B gene in a stool sample and is highly accurate.
- GDH/EIA. Some hospitals use a glutamate dehydrogenase (GDH) test in conjunction with an enzyme immunoassay (EIA) test. GDH is a very sensitive assay and can accurately rule out the presence of C. difficile in stool samples.
- Enzyme immunoassay. The enzyme immunoassay (EIA) test is faster than other tests but isn't sensitive enough to detect many infections and has a higher rate of falsely normal results. This is typically not the only test used.
- Cell cytotoxicity assay. A cytotoxicity test looks for the effects of the C. difficile toxin on human cells grown in a culture. This type of test is sensitive, but it is less widely available, is more cumbersome to do and requires 24 to 48 hours for test results. It's typically used in research settings.
Testing for C. difficile is unnecessary if you're not having diarrhea or watery stools, and isn't helpful for follow-up treatment. If you aren't having diarrhea, stool shouldn't be tested for C. difficile.
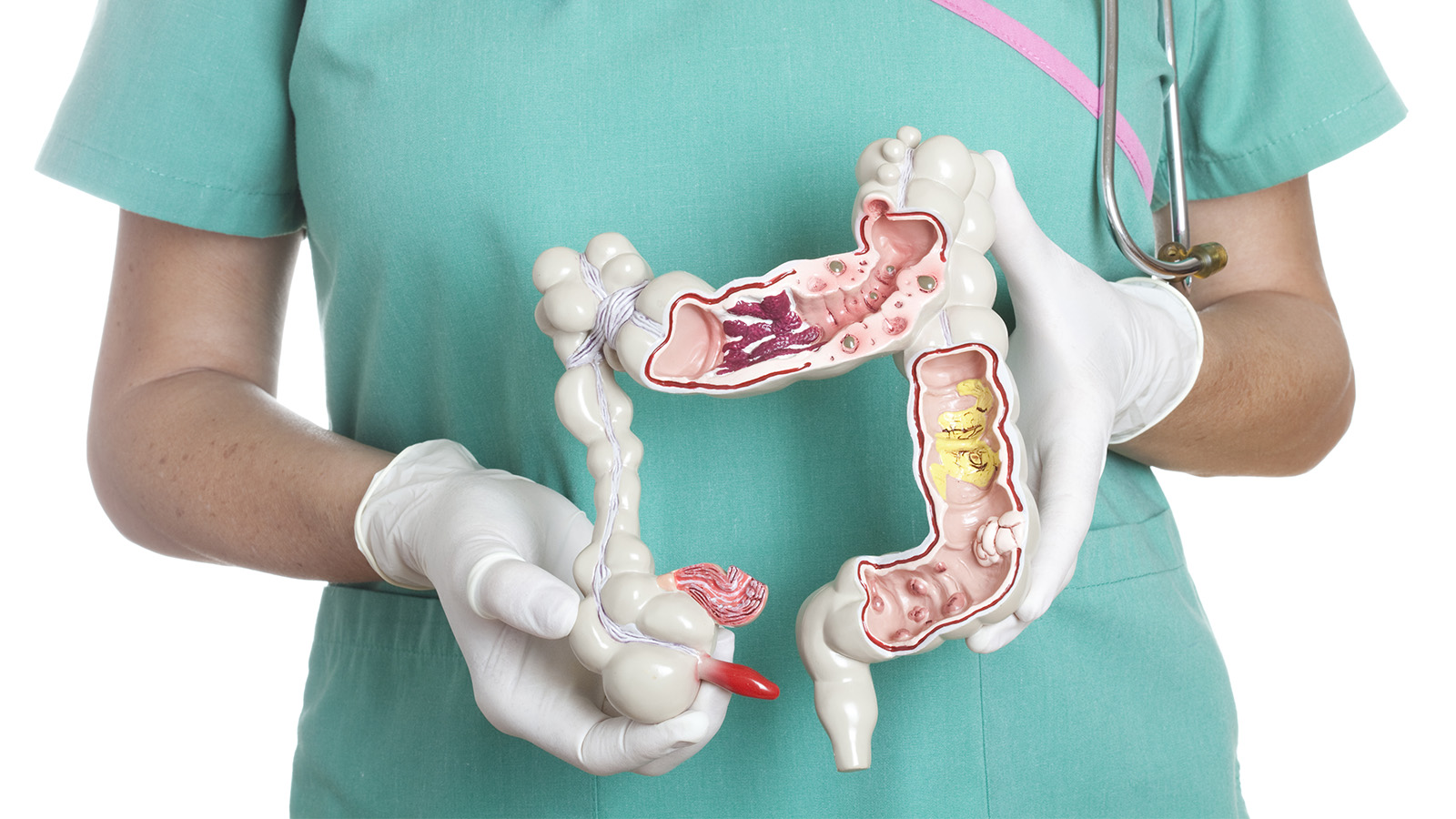
2. Colon examination
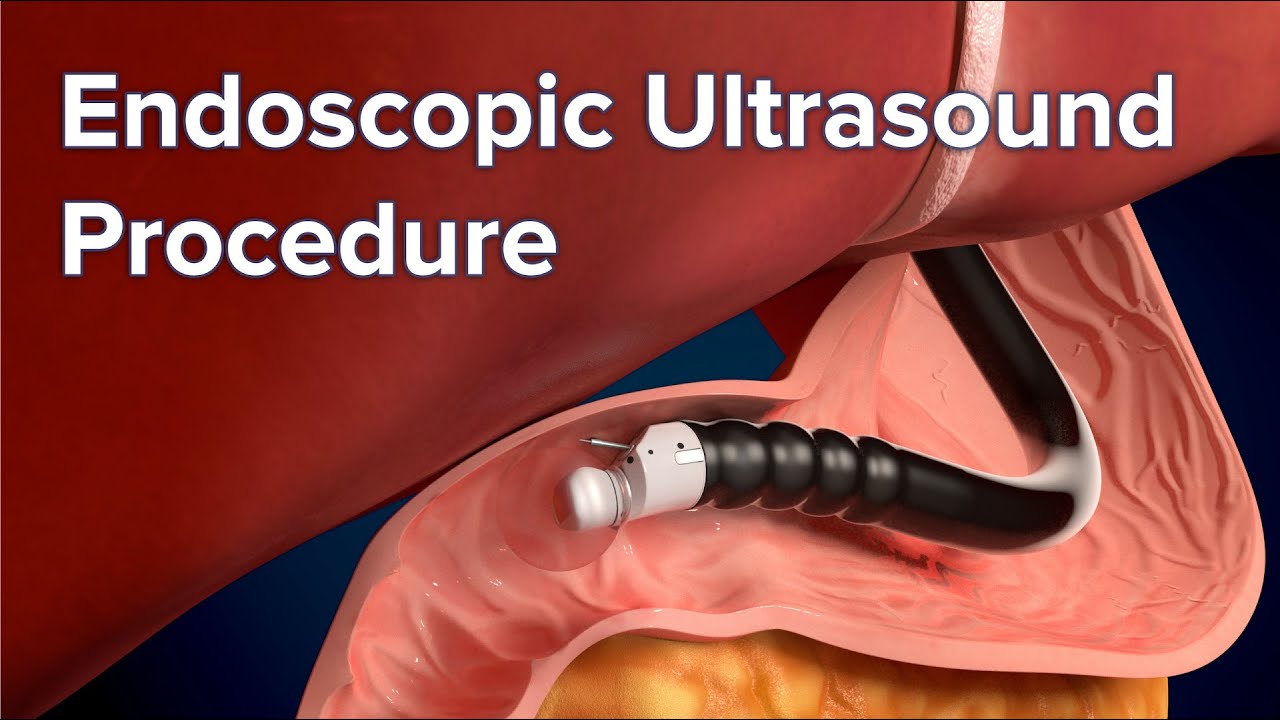
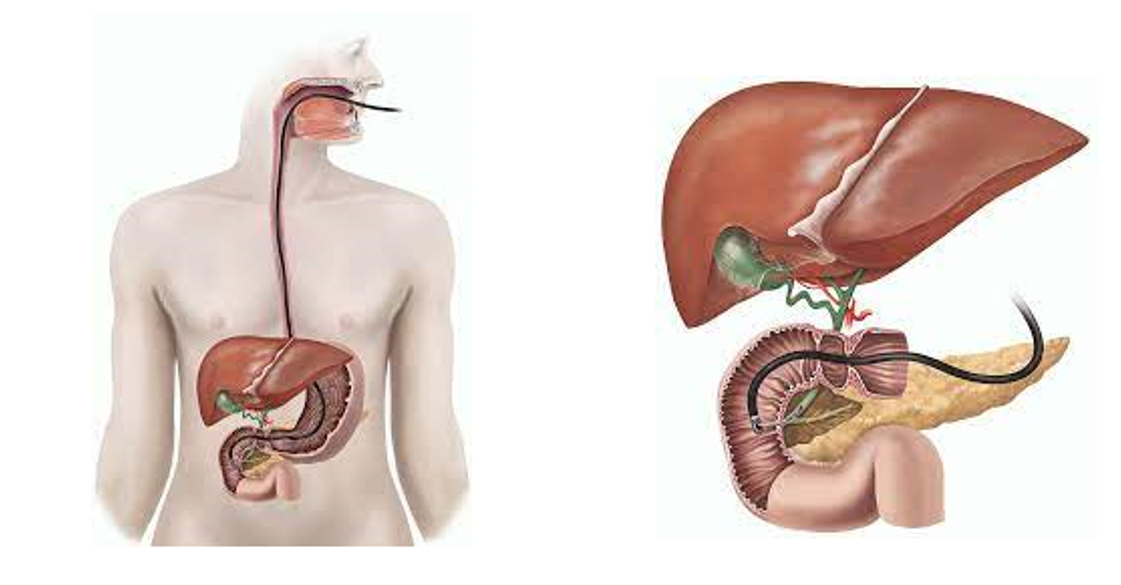
In rare instances, to help confirm a diagnosis of C. difficile infection and look for alternative causes of your symptoms, your doctor may examine the inside of your colon. This test (flexible sigmoidoscopy or colonoscopy) involves inserting a flexible tube with a small camera on one end into your colon to look for areas of inflammation and pseudomembranes.
3. Imaging tests
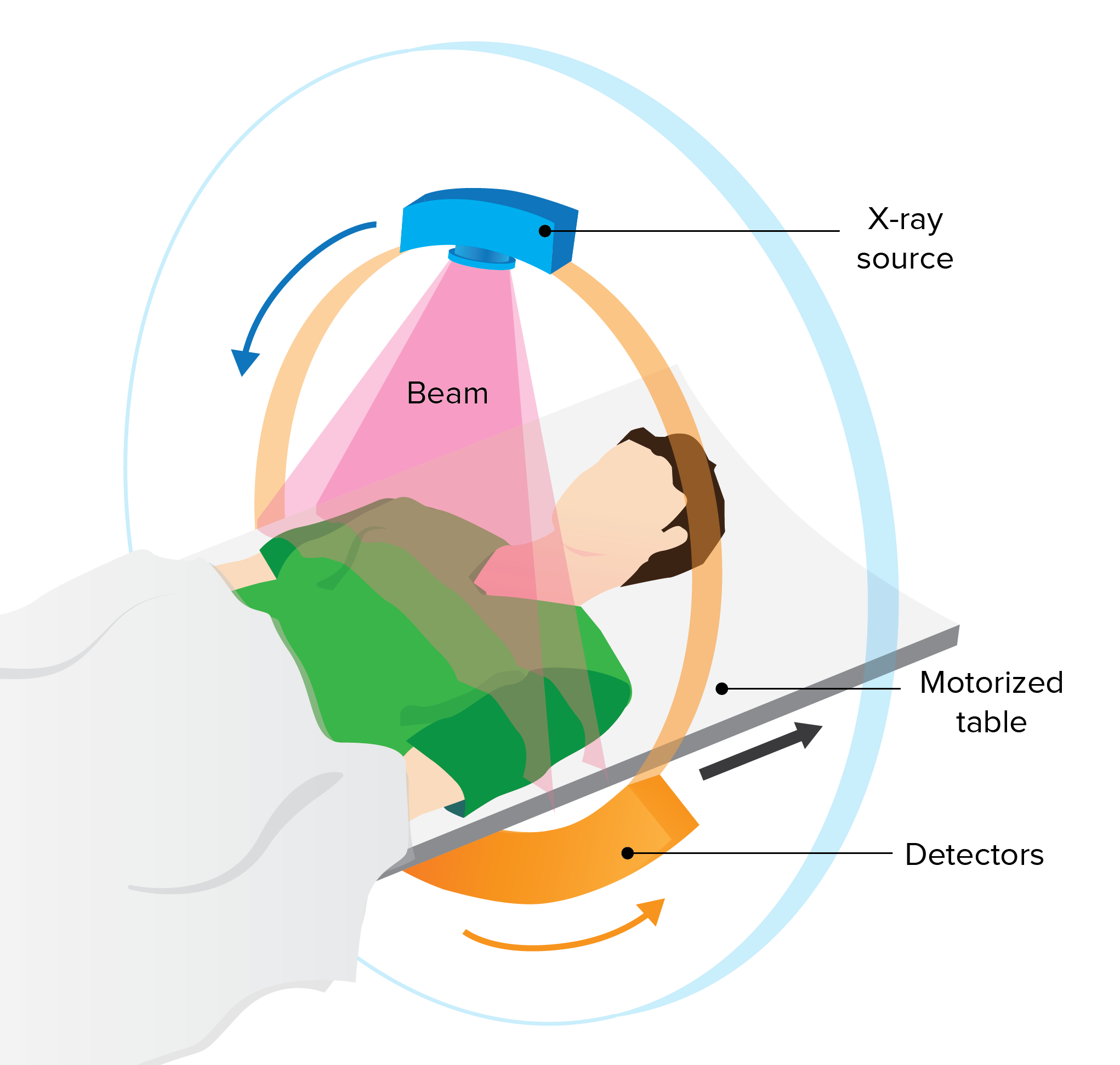
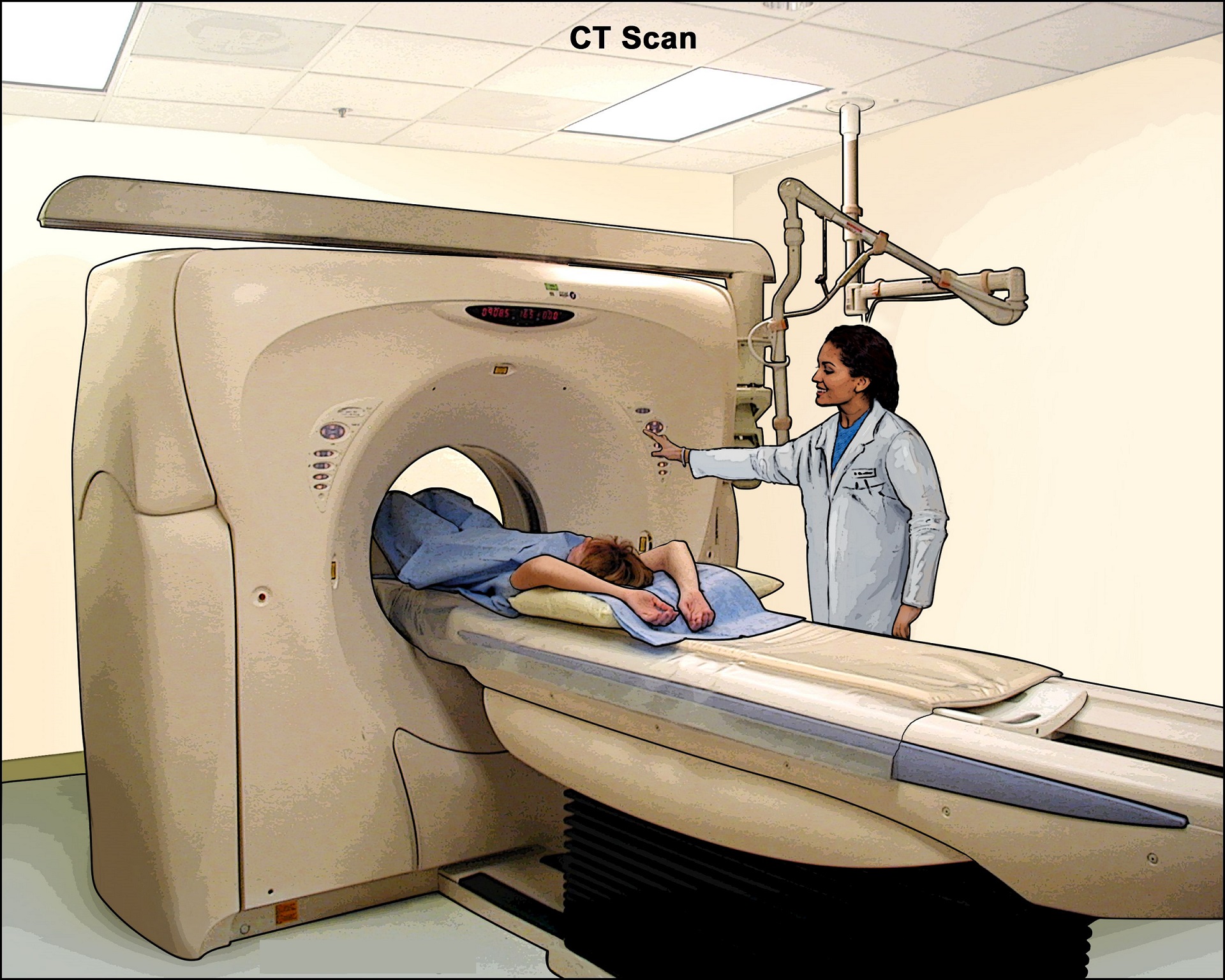
If your doctor is concerned about possible complications of C. difficile, he or she may order an abdominal X-ray or a computerized tomography (CT) scan, which provides images of your colon. The scan can detect the presence of complications such as thickening of the colon wall, expansion of the bowel or, more rarely, a hole (perforation) in the lining of your colon.
Treatment
The first step in treating C. difficile is to stop taking the antibiotic that triggered the infection, when possible. Depending on the severity of your infection, treatment may include:
- Antibiotics. Ironically, the standard treatment for C. difficile is another antibiotic. These antibiotics keep C. difficile from growing, which in turn treats diarrhea and other complications. Your doctor may prescribe vancomycin (Vancocin HCL, Firvanq) or fidaxomicin (Dificid).
Metronidazole (Flagyl) may be rarely used if vancomycin or fidaxomicin aren't available. - Surgery. For people who have severe pain, organ failure, toxic megacolon or inflammation of the lining of the abdominal wall, surgery to remove the diseased portion of the colon may be the only option.
Recurrent infection
Up to 20% (Source) of people with C. difficile get sick again, either because the initial infection never went away or because they've been reinfected with a different strain of the bacteria.
Your risk of recurrence is higher if you:
- Are older than 65
- Are taking other antibiotics for a different condition while being treated with antibiotics for C. difficile infection
- Have a severe underlying medical disorder, such as chronic kidney failure, inflammatory bowel disease or chronic liver disease
Treatment for Recurrent Disease may include:
- Antibiotics. Antibiotic therapy for recurrence may involve one or more courses of a medication. In general, guidelines recommend not repeating the same therapy used for an initial infection for a recurrent infection. The effectiveness of antibiotic therapy declines with each subsequent recurrence.
- Fecal microbiota transplant (FMT). Also known as a stool transplant, FMT is emerging as an alternative strategy for treating recurrent C. difficile infections. Though FMT is considered experimental and is not yet approved by the FDA, clinical studies are currently underway.
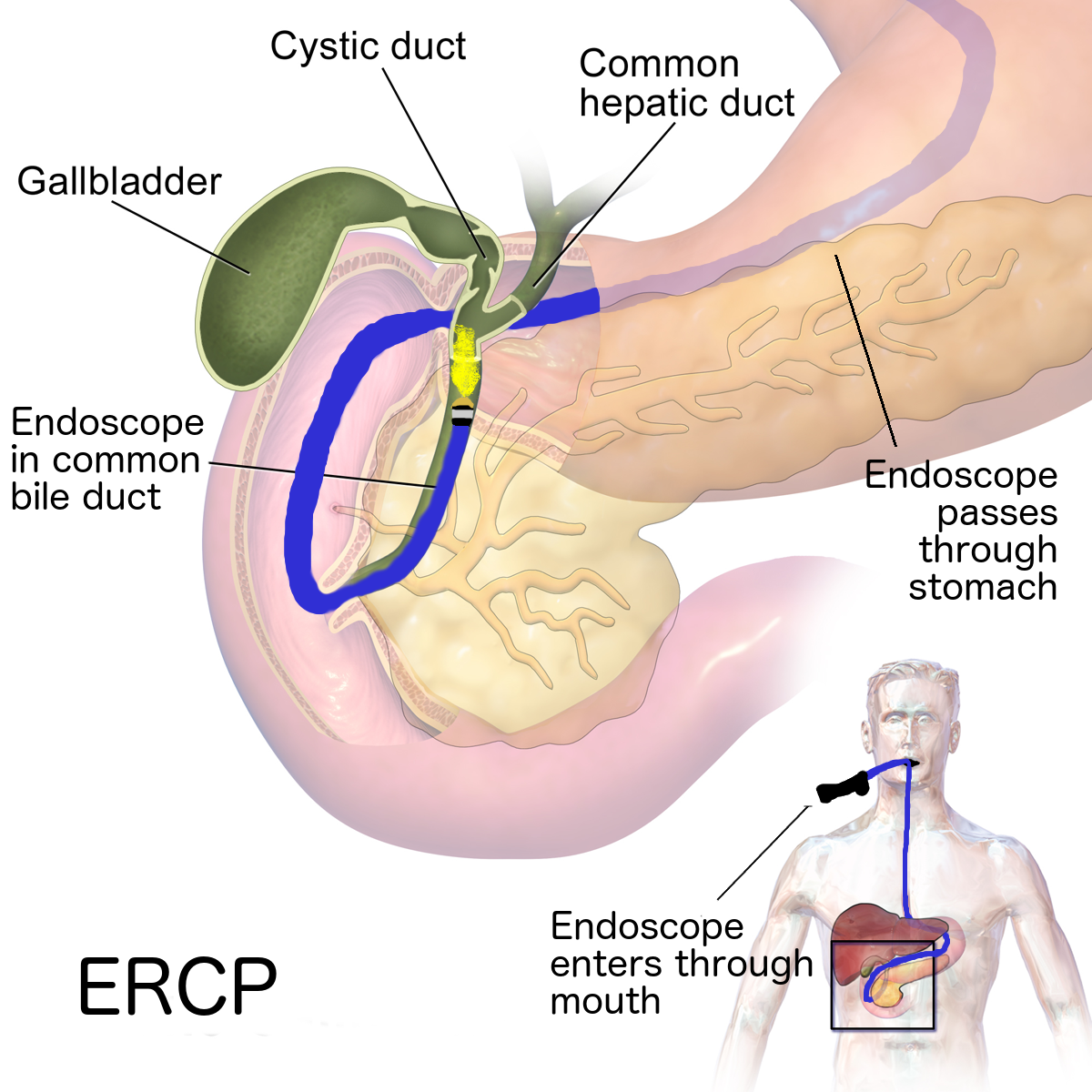
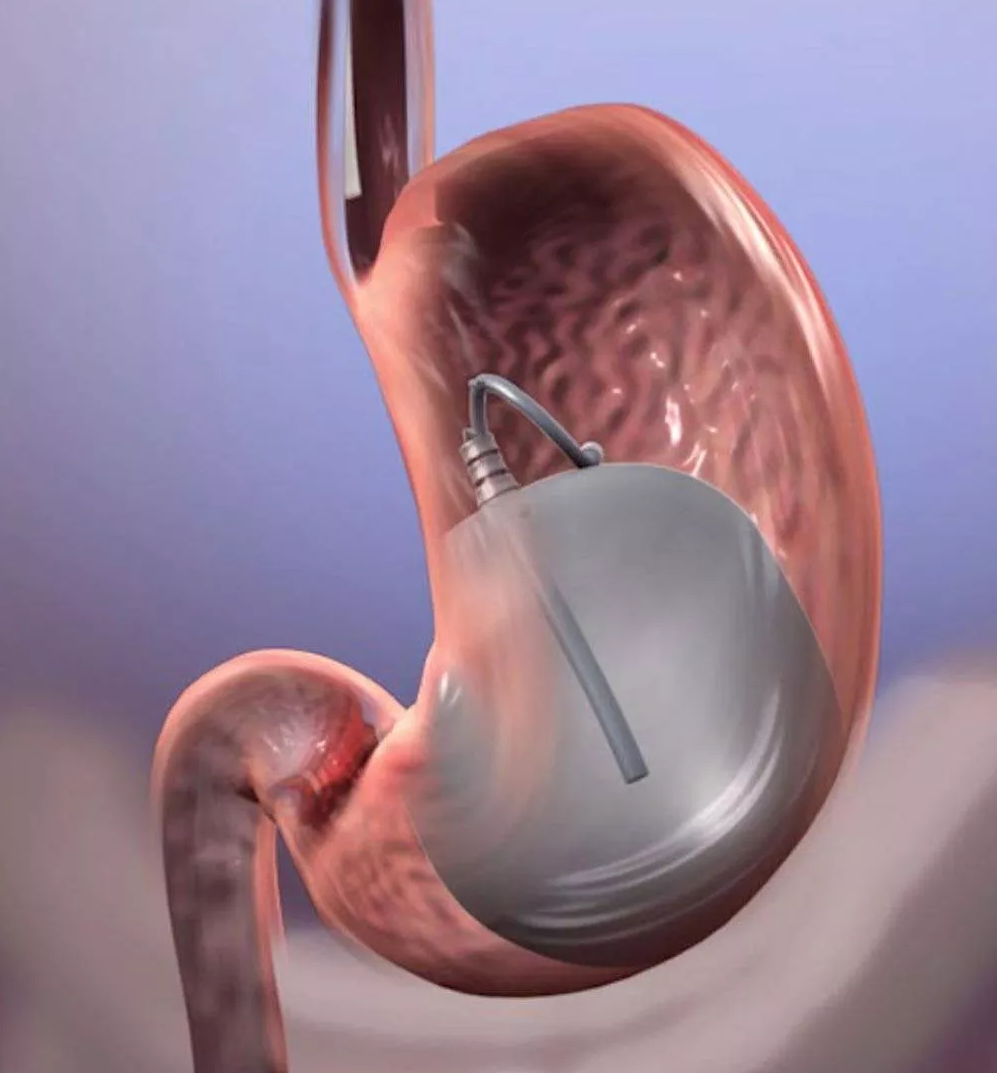
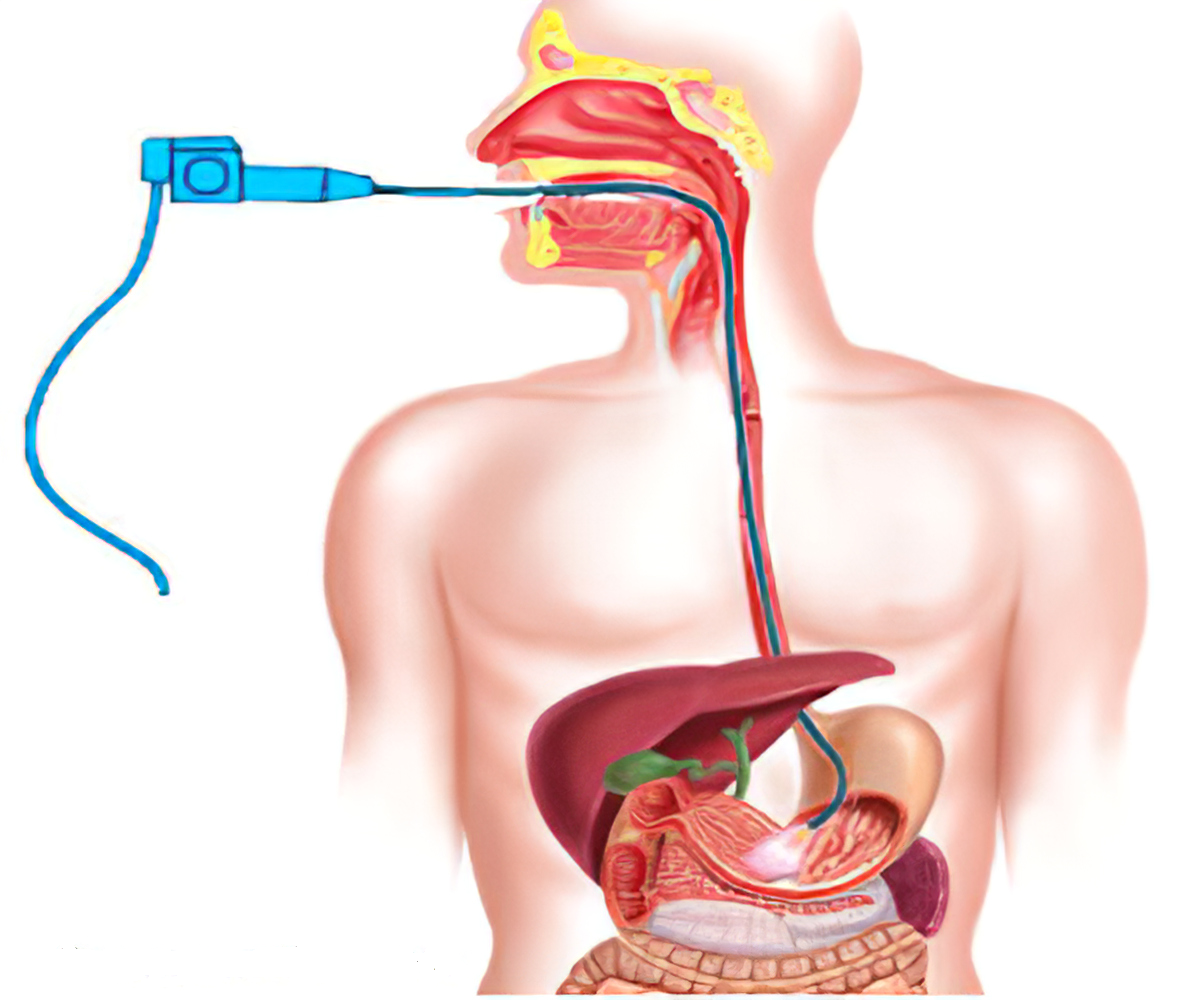
FMT restores healthy intestinal bacteria by placing another person's (donor's) stool in your colon through a colonoscope or nasogastric tube. Donors are screened for medical conditions, their blood is tested for infections, and stools are carefully screened for parasites, viruses and other infectious bacteria before being used for FMT.
Research has shown that FMT done one or more times has a success rate higher than 85% for treating C. difficile infections. - Probiotics. Probiotics are organisms, such as bacteria and yeast, and are available over the counter. The role of these products in C. difficile infection is controversial. Research hasn't consistently shown that currently available products are helpful in preventing or treating infection with C. difficile. Advanced probiotics are currently being studied for their potential use in C. difficile treatment or prevention but aren't currently available.