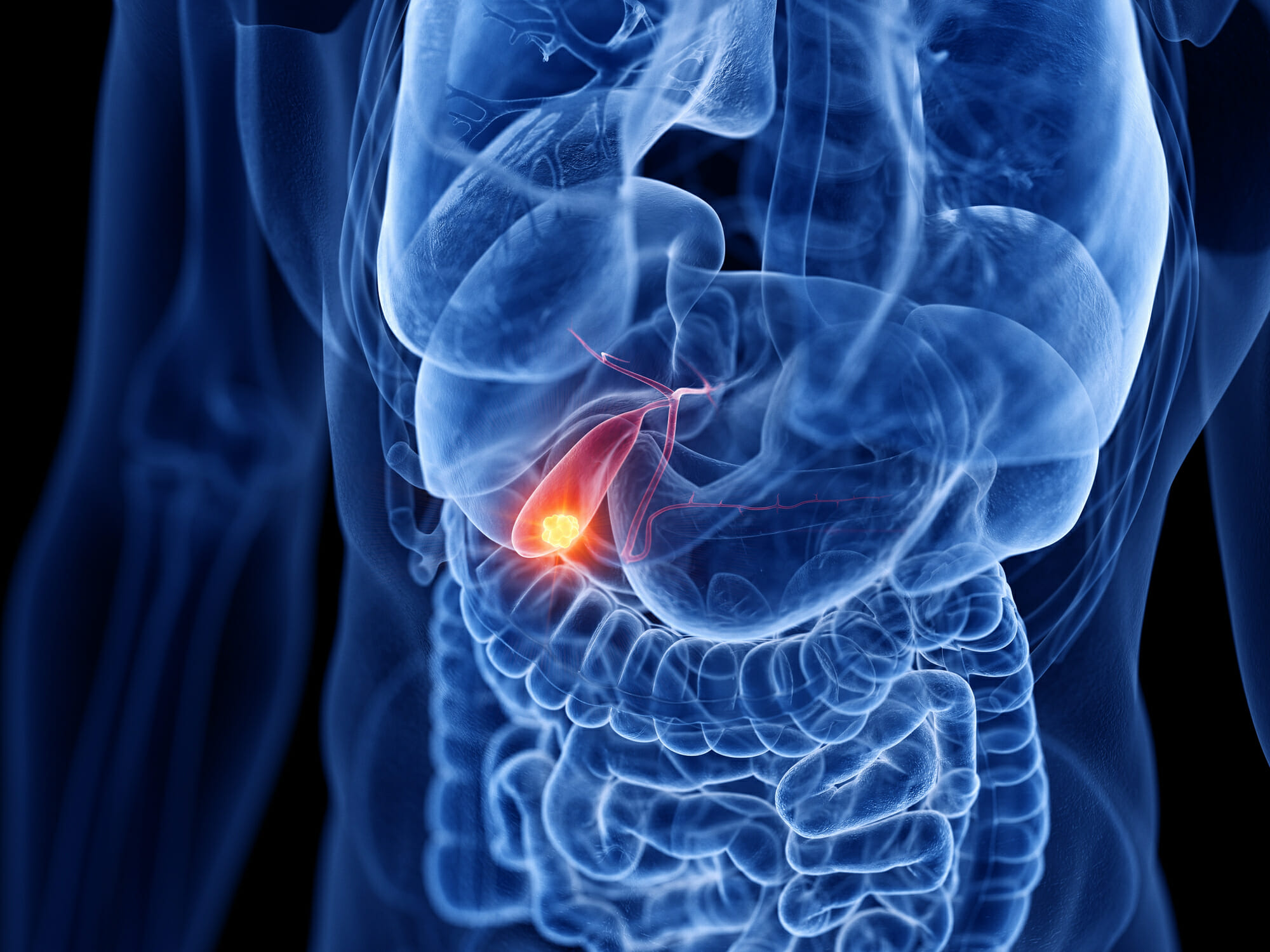
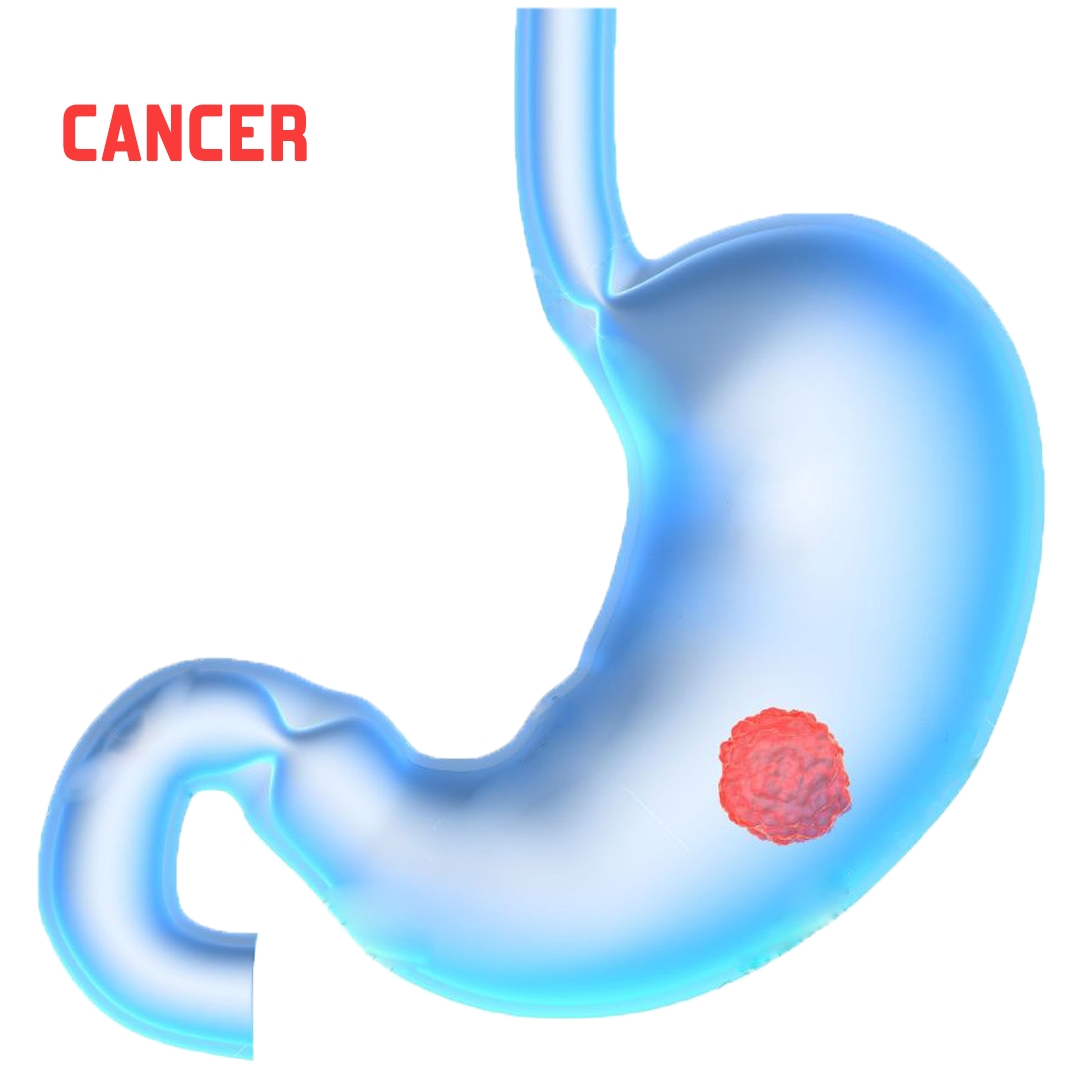
Colon Cancer
6 Ways to Prevent Colon Cancer
Colon cancer can be a devastating diagnosis, but there are a number of steps you can take to reduce your risk of tumors, as experts say.
Overview
Colorectal cancer (CRC) is a formidable health problem worldwide. It is the third most common cancer in men (663000 cases, 10.0% of all cancer cases) and the second most common in women (571000 cases, 9.4% of all cancer cases). The number of CRC-related deaths is estimated to be approximately 608000 worldwide, accounting for 8% of all cancer deaths and making CRC the fourth most common cause of death due to cancer. (Source)
While a person is healthy, they rarely think about preventing any illness. But as the saying goes, prevention is better than cure, it is best to know about the risk factors and how we can reduce the chances of colorectal cancer.
As part of Colorectal Cancer Awareness Month in March, we are highlighting the risk factors of colorectal cancer and how we can reduce these risks.
Risk Factors
Studies have found the following risk factors for colorectal cancer:
- Age over 50: Colorectal cancer is more likely to occur as people get older. More than 90 percent of people with this disease are diagnosed after age 50. The average age at diagnosis is 72.
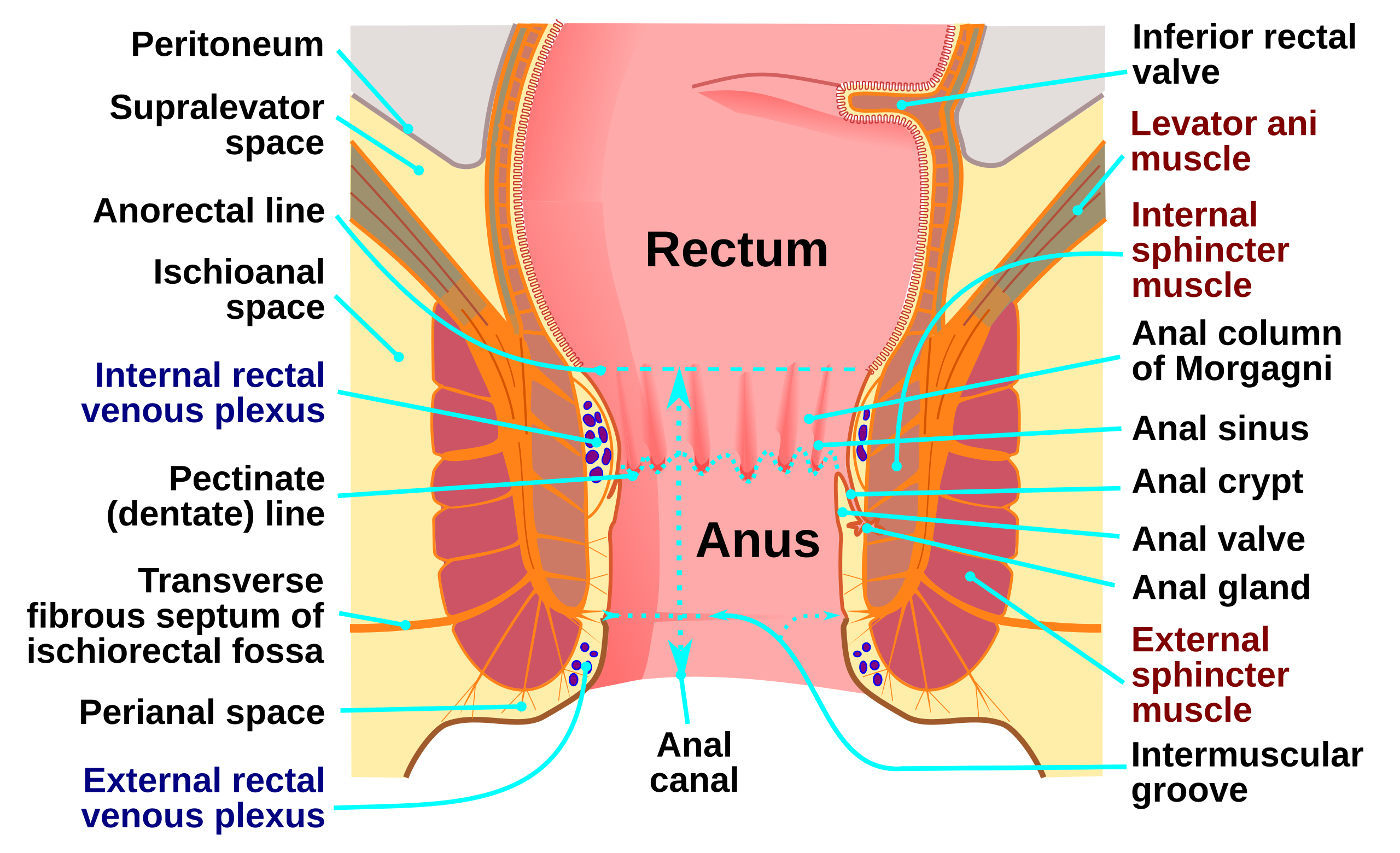
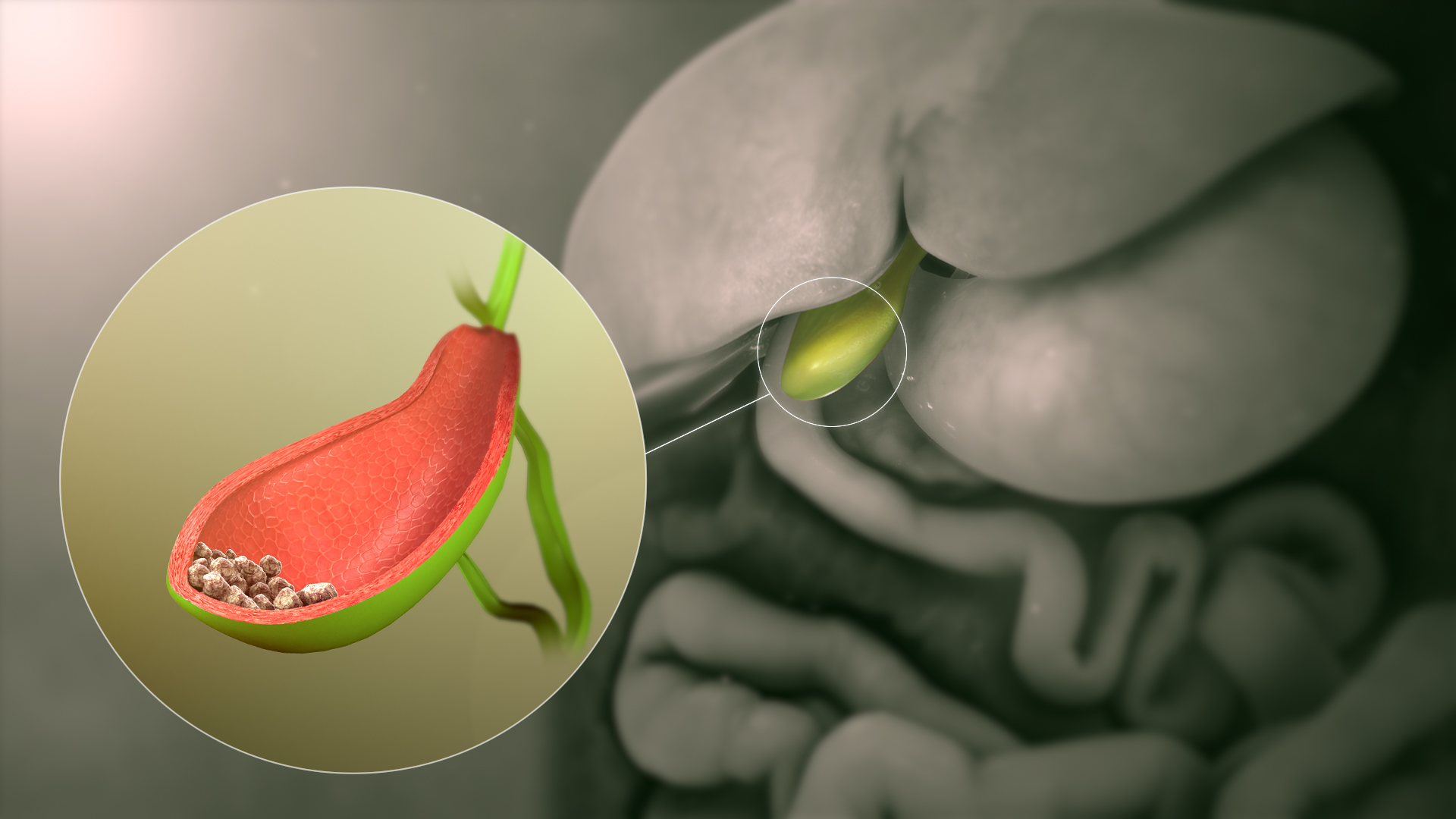
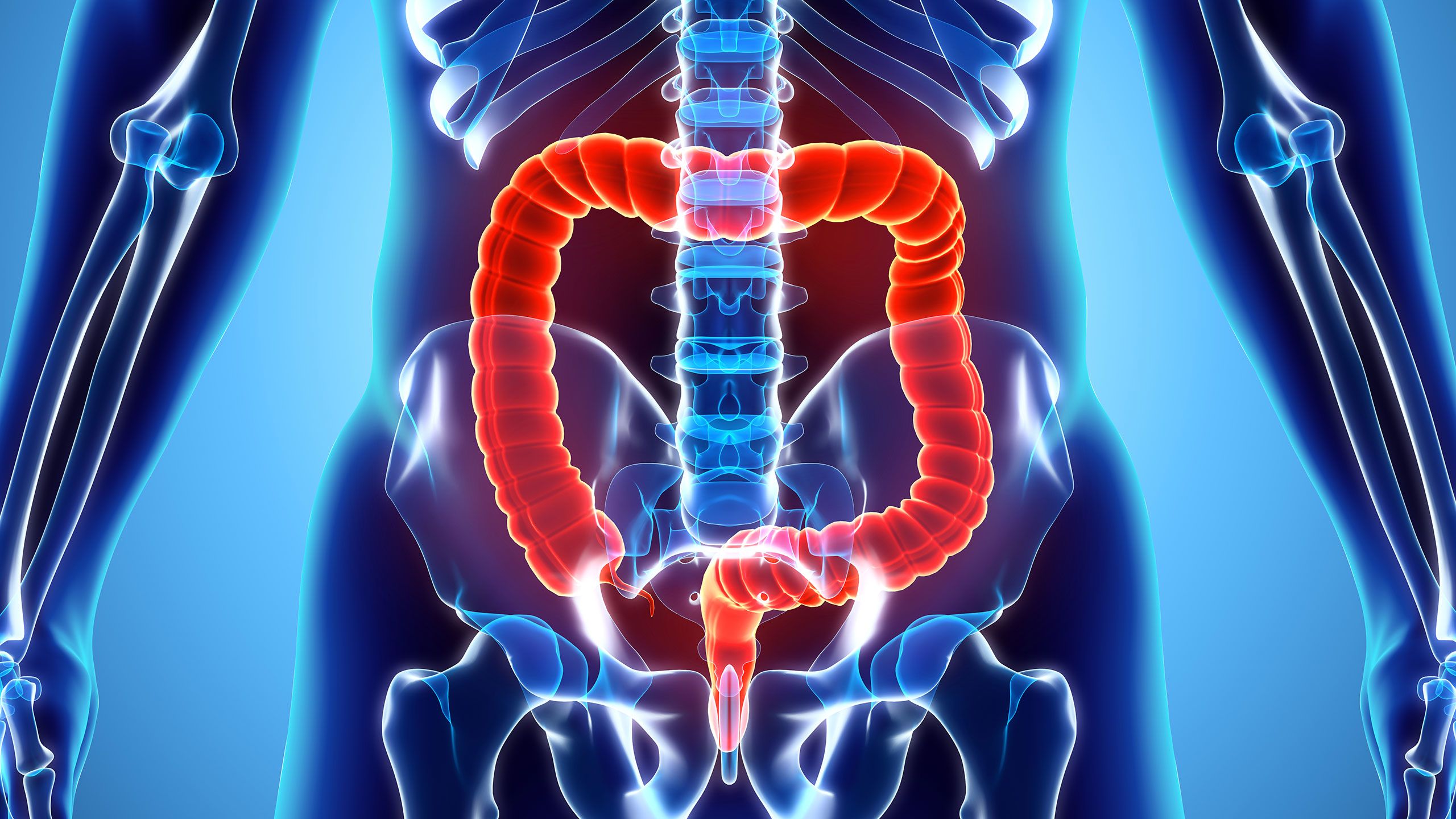
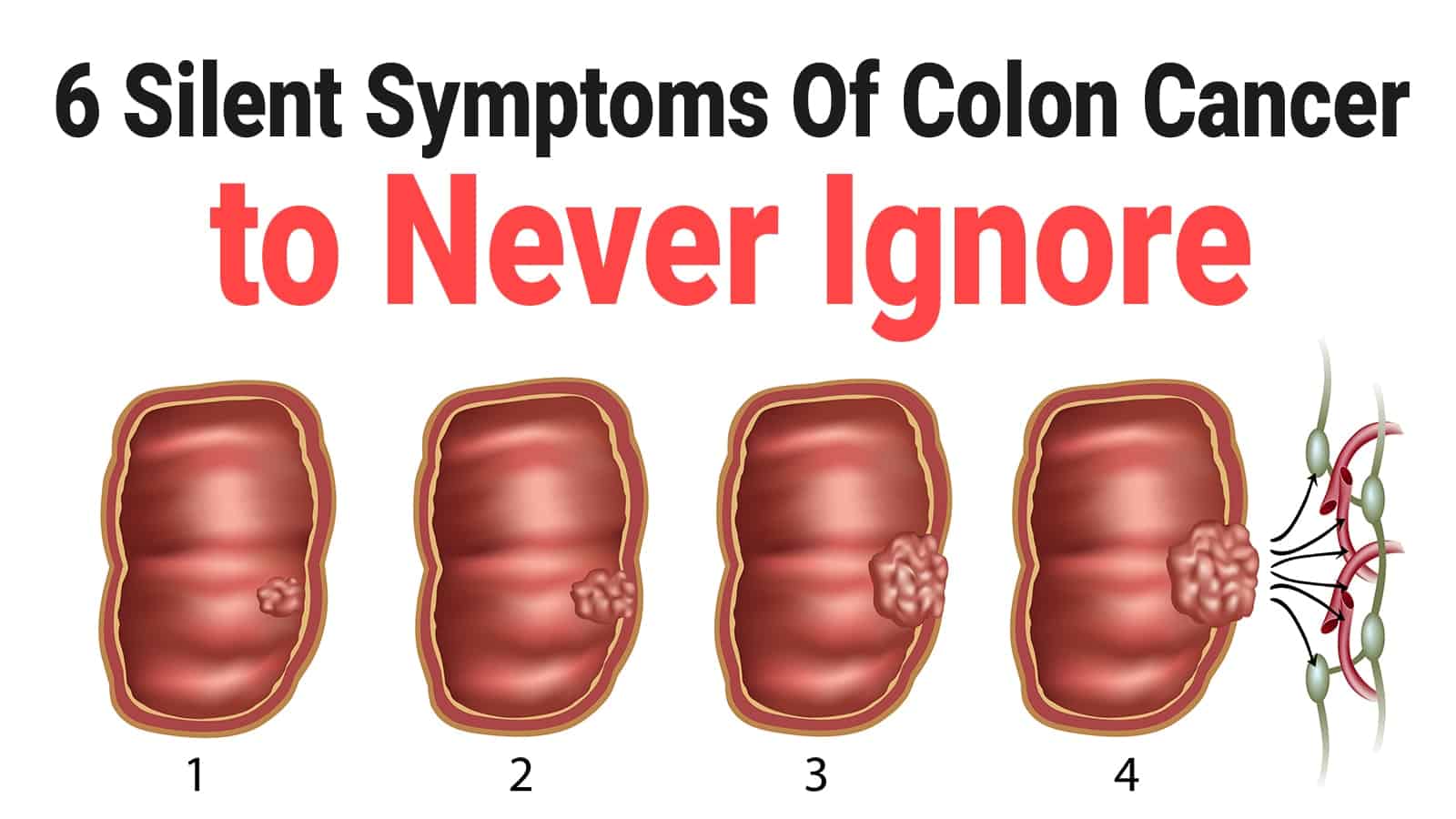
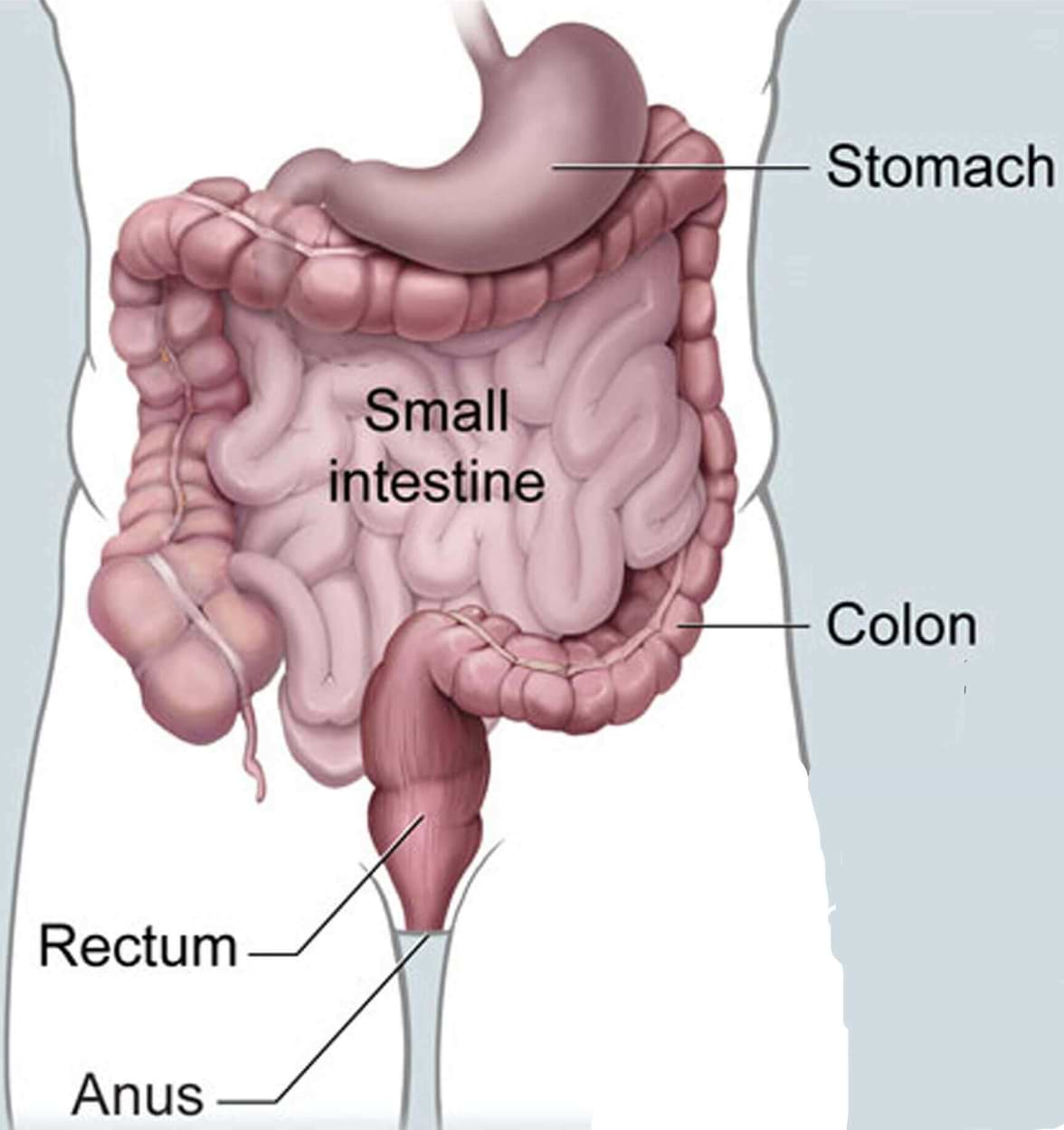
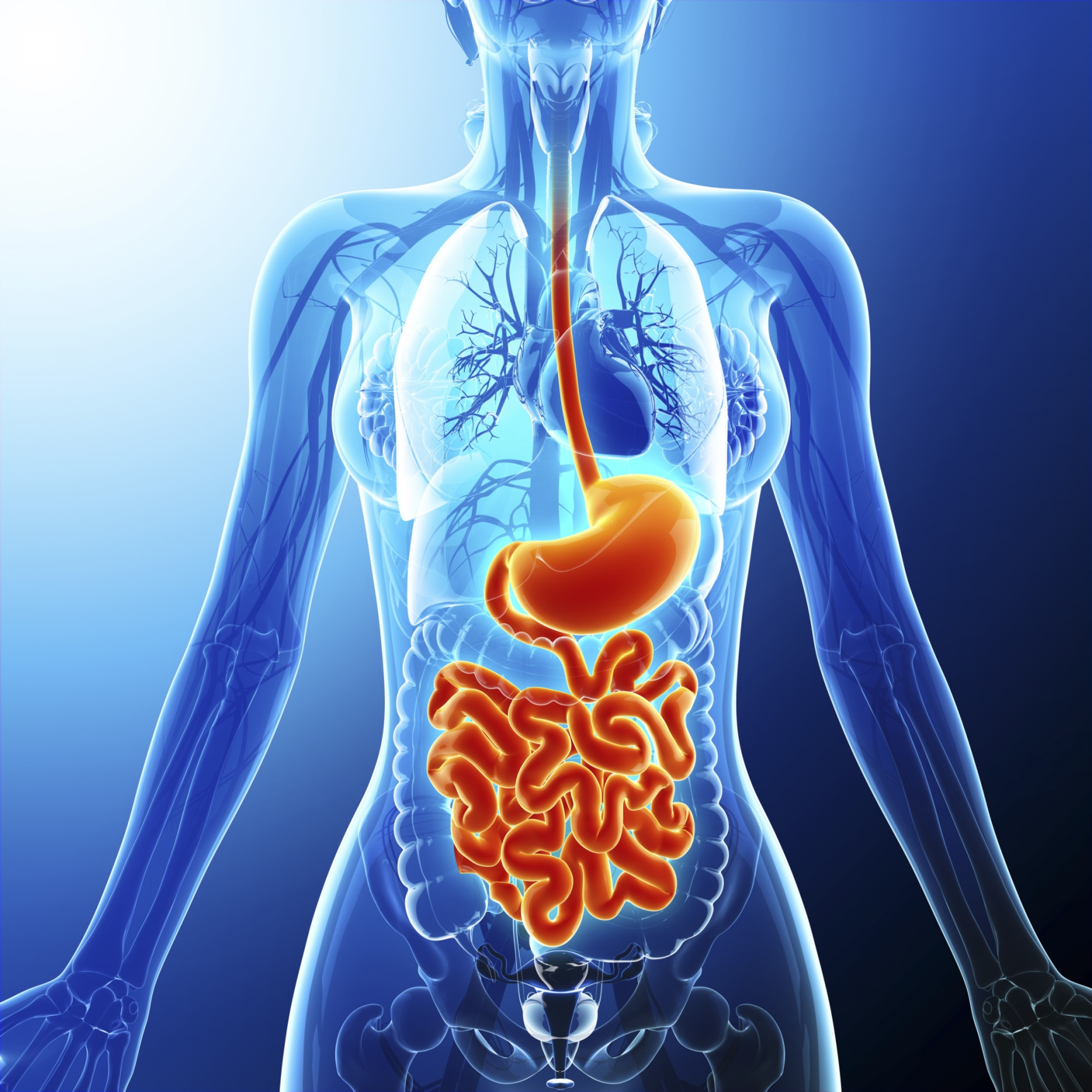
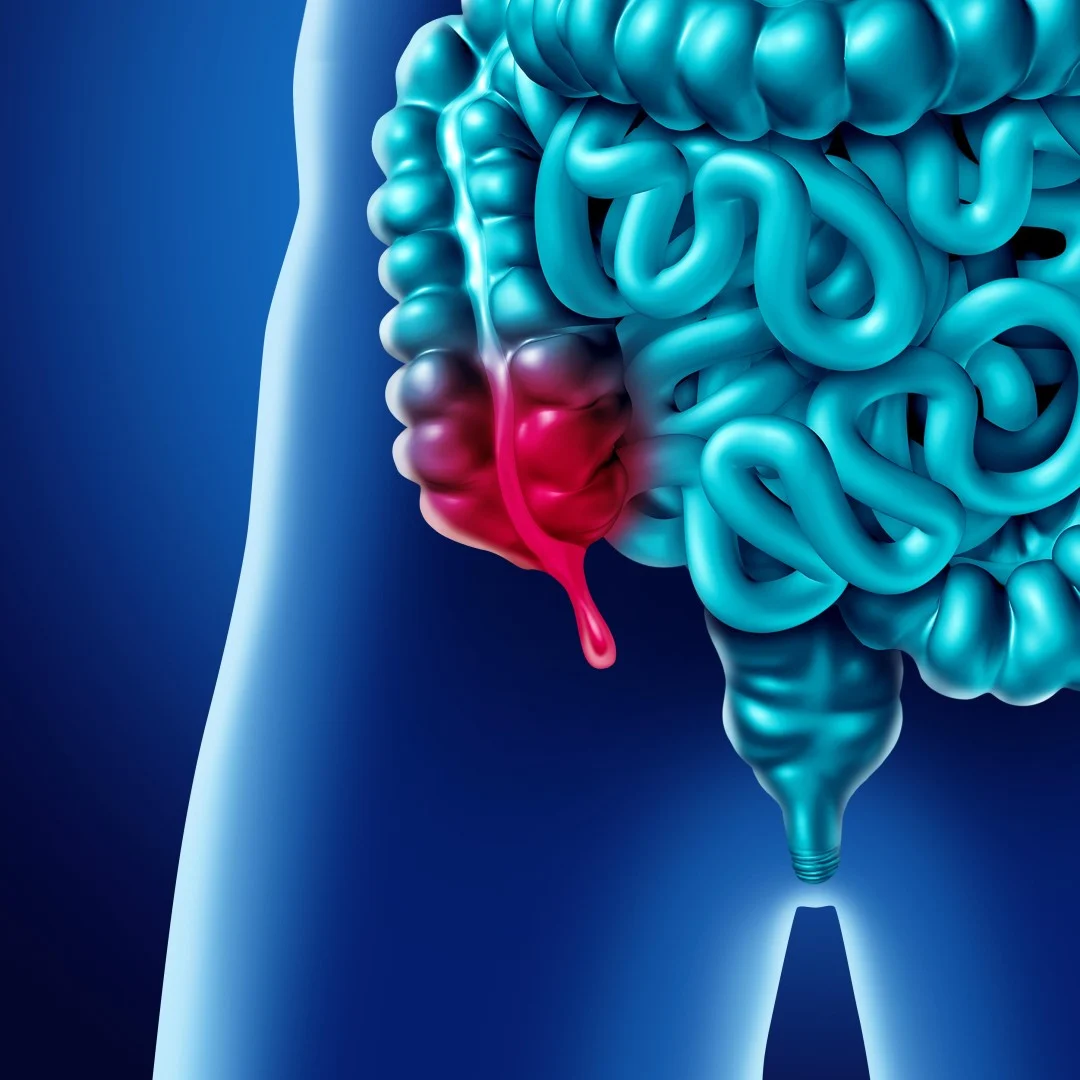
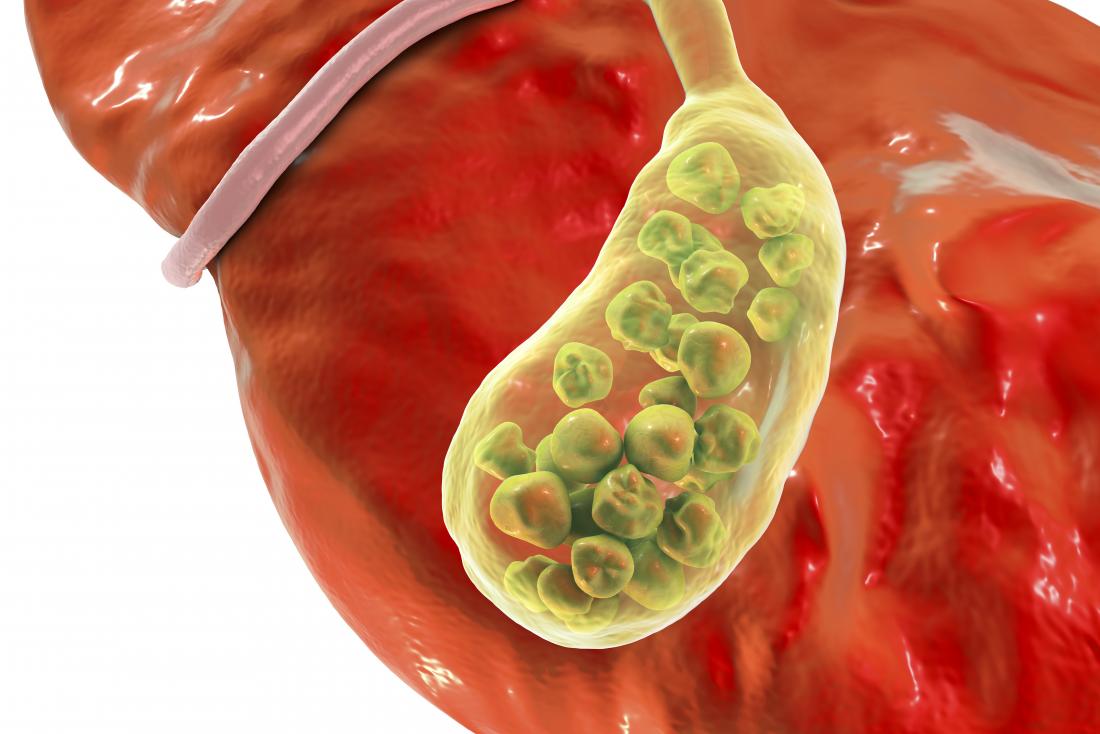
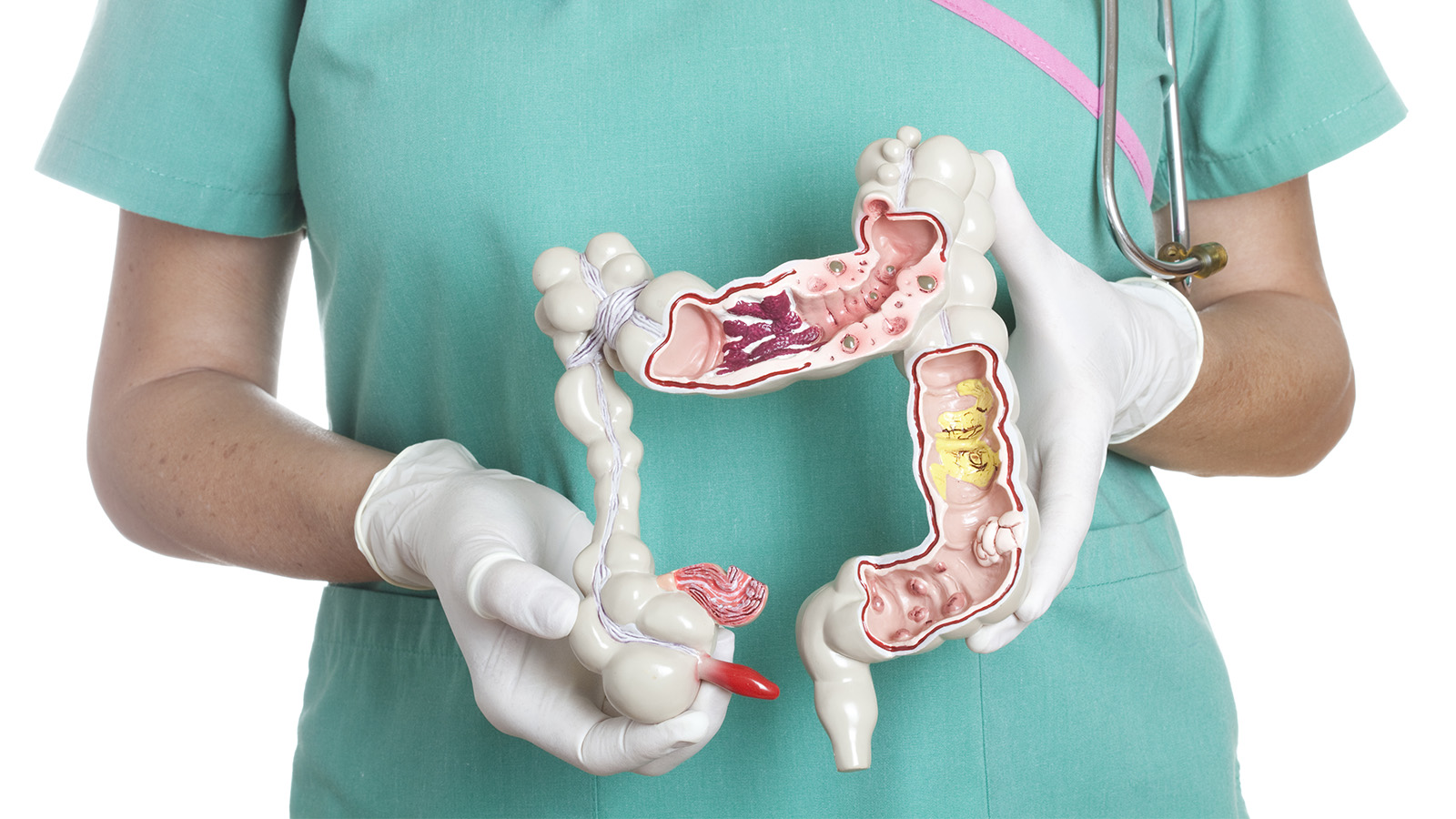
- Colorectal polyps: Polyps are growths on the inner wall of the colon or rectum. They are common in people over age 50. Most polyps are benign (not cancer), but some polyps (adenomas) can become cancer. Finding and removing polyps may reduce the risk of colorectal cancer.
- Family history of colorectal cancer: Close relatives (parents, brothers, sisters, or children) of a person with a history of colorectal cancer are somewhat more likely to develop this disease themselves, especially if the relative had the cancer at a young age. If many close relatives have a history of colorectal cancer, the risk is even greater.
- Genetic alterations: Changes in certain genes increase the risk of colorectal cancer.
- Hereditary nonpolyposis colon cancer (HNPCC) is the most common type of inherited (genetic) colorectal cancer. It accounts for about 2 percent of all colorectal cancer cases. It is caused by changes in an HNPCC gene. Most people with an altered HNPCC gene develop colon cancer, and the average age at diagnosis of colon cancer is 44.
- Familial adenomatous polyposis (FAP) is a rare, inherited condition in which hundreds of polyps form in the colon and rectum. It is caused by a change in a specific gene called APC. Unless FAP is treated, it usually leads to colorectal cancer by age 40. FAP accounts for less than 1 percent of all colorectal cancer cases.
Family members of people who have HNPCC or FAP can have genetic testing to check for specific genetic changes. For those who have changes in their genes, health care providers may suggest ways to try to reduce the risk of colorectal cancer, or to improve the detection of this disease. For adults with FAP, the doctor may recommend an operation to remove all or part of the colon and rectum.
- Personal history of cancer: A person who has already had colorectal cancer may develop colorectal cancer a second time. Also, women with a history of cancer of the ovary, uterus (endometrium), or breast are at a somewhat higher risk of developing colorectal cancer.
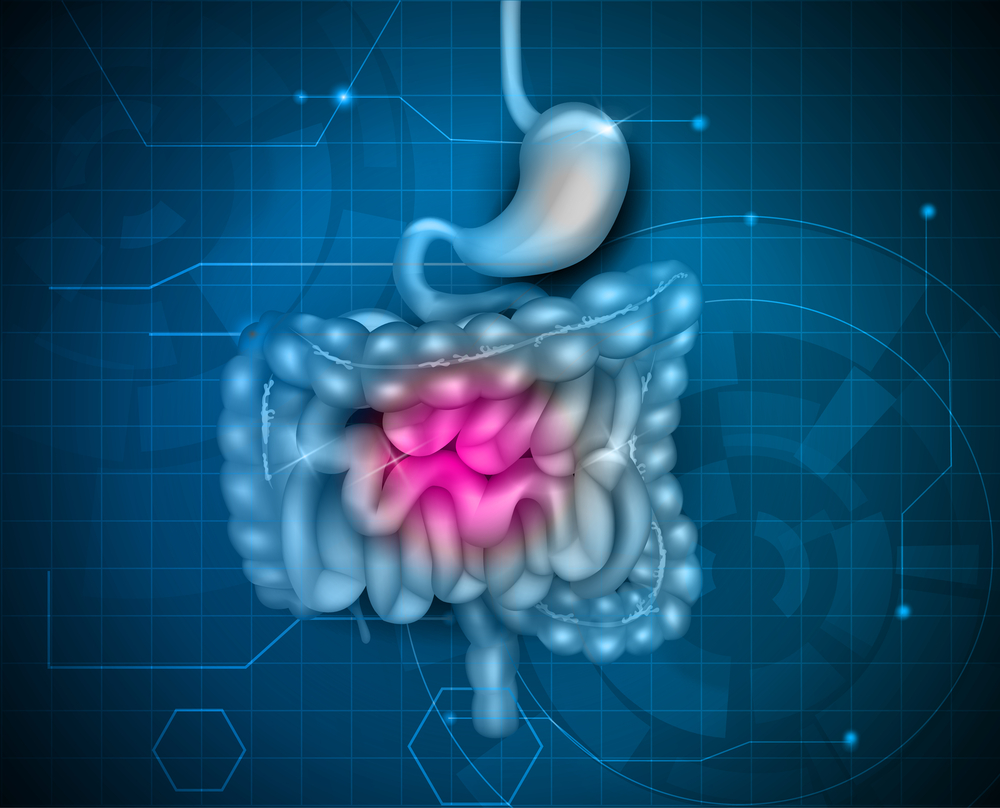
- Ulcerative colitis or Crohn disease: A person who has had a condition that causes inflammation of the colon (such as ulcerative colitis or Crohn's disease) for many years is at increased risk of developing colorectal cancer.
- Diet: Studies suggest that diets high in fat (especially animal fat) and low in calcium, folate, and fiber may increase the risk of colorectal cancer. Also, some studies suggest that people who eat a diet very low in fruits and vegetables may have a higher risk of colorectal cancer. However, results from diet studies do not always agree, and more research is needed to better understand how diet affects the risk of colorectal cancer.
- Cigarette smoking: A person who smokes cigarettes may be at increased risk of developing polyps and colorectal cancer.
Because people who have colorectal cancer may develop colorectal cancer a second time, it is important to have checkups. If you have colorectal cancer, you also may be concerned that your family members may develop the disease. People who think they may be at risk should talk to their doctor. The doctor may be able to suggest ways to reduce the risk and can plan an appropriate schedule for checkups. See the "Screening" section to learn more about tests that can find polyps or colorectal cancer.
Reducing the risk of COlorectal Cancer
Get screened
When detected early, colorectal cancer is highly treatable. Adults at average risk for colorectal cancer should begin screening at age 45, while those with parents, grandparents and siblings who have had colorectal cancer should begin screening at age 40, or 10 years before the diagnosis of the youngest first-degree relative.
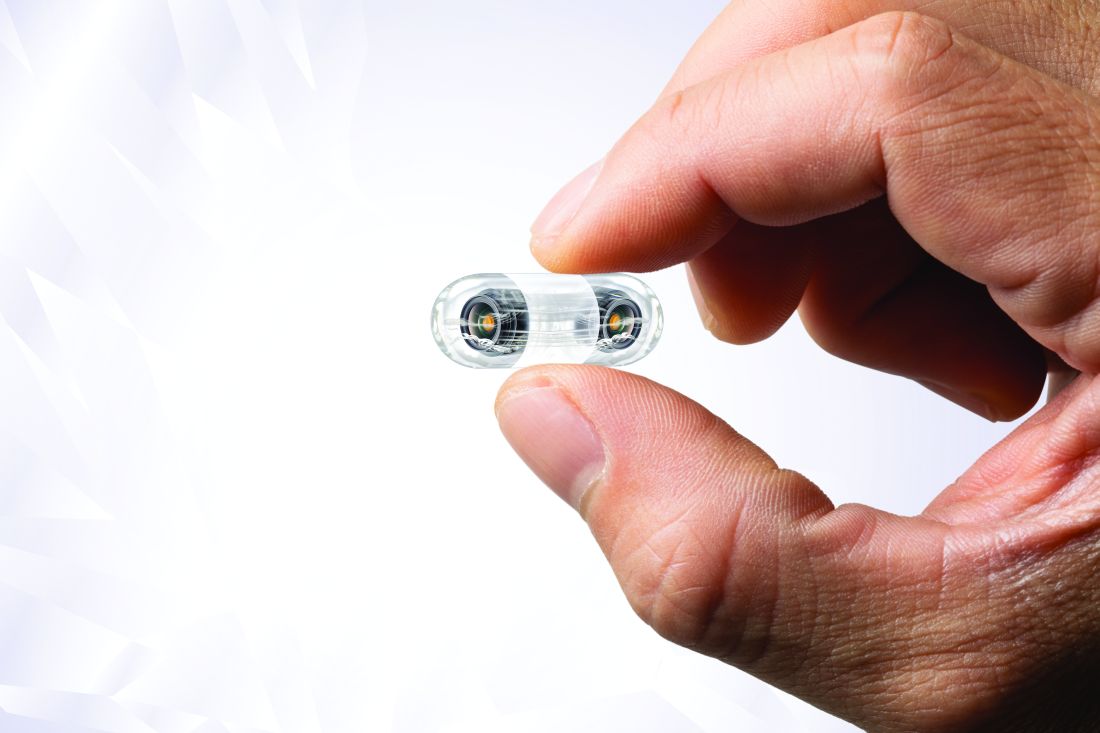
Several screening tests can be used to find polyps or colorectal cancer. The Task Force outlines the following colorectal cancer screening strategies. It is important to know that if your test result is positive or abnormal on some screening tests (stool tests, flexible sigmoidoscopy, and CT colonography), a colonoscopy test is needed to complete the screening process. Talk to your doctor about which test is right for you.
Stool Tests
- The guaiac-based fecal occult blood test (gFOBT) uses the chemical guaiac to detect blood in the stool. It is done once a year. For this test, you receive a test kit from your health care provider. At home, you use a stick or brush to obtain a small amount of stool. You return the test kit to the doctor or a lab, where the stool samples are checked for the presence of blood.
- The fecal immunochemical test (FIT) uses antibodies to detect blood in the stool. It is also done once a year in the same way as a gFOBT.
- The FIT-DNA test (also referred to as the stool DNA test) combines the FIT with a test that detects altered DNA in the stool. For this test, you collect an entire bowel movement and send it to a lab, where it is checked for altered DNA and for the presence of blood. It is done once every three years.
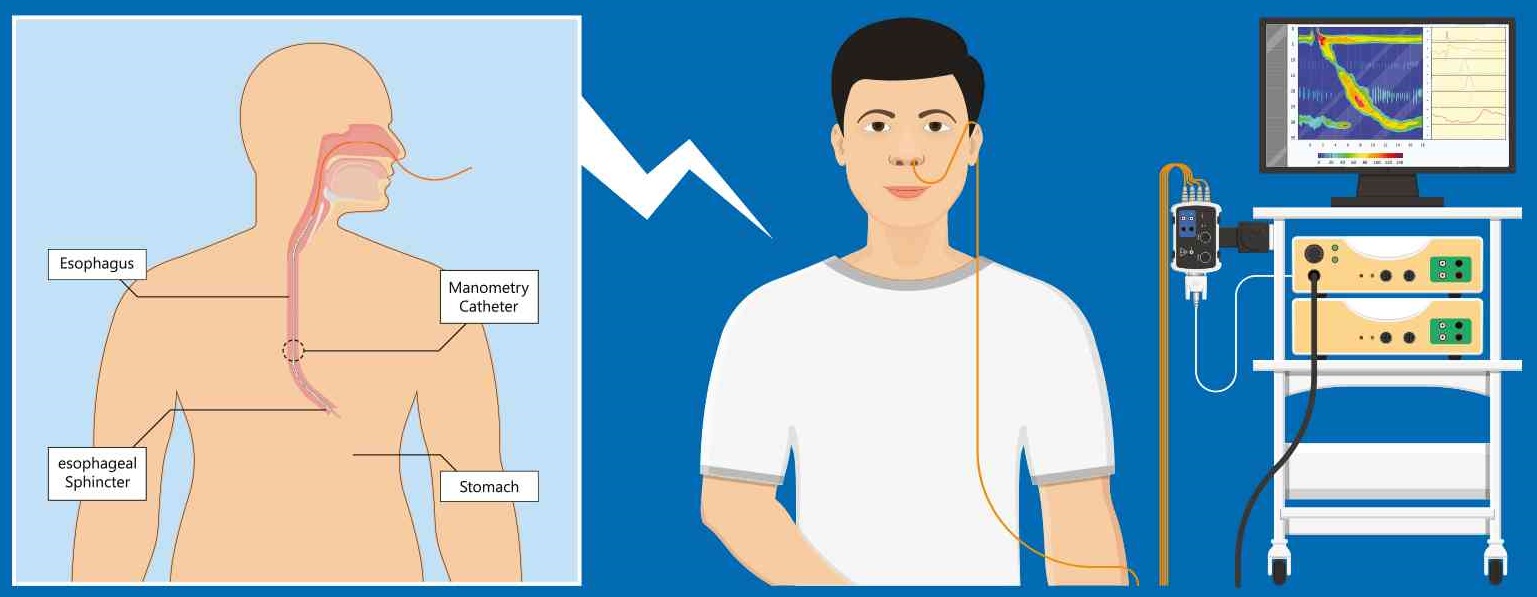
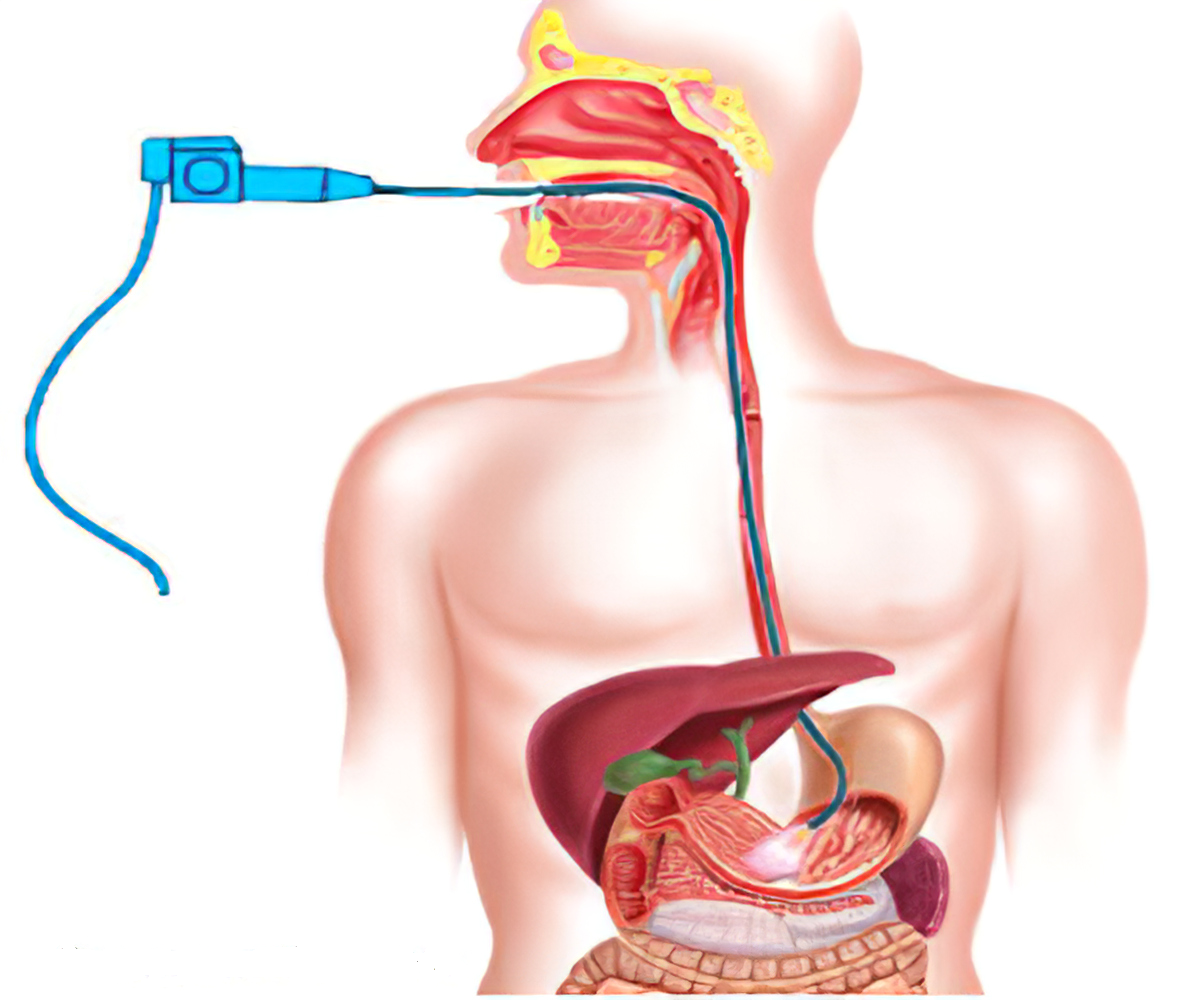
Flexible Sigmoidoscopy
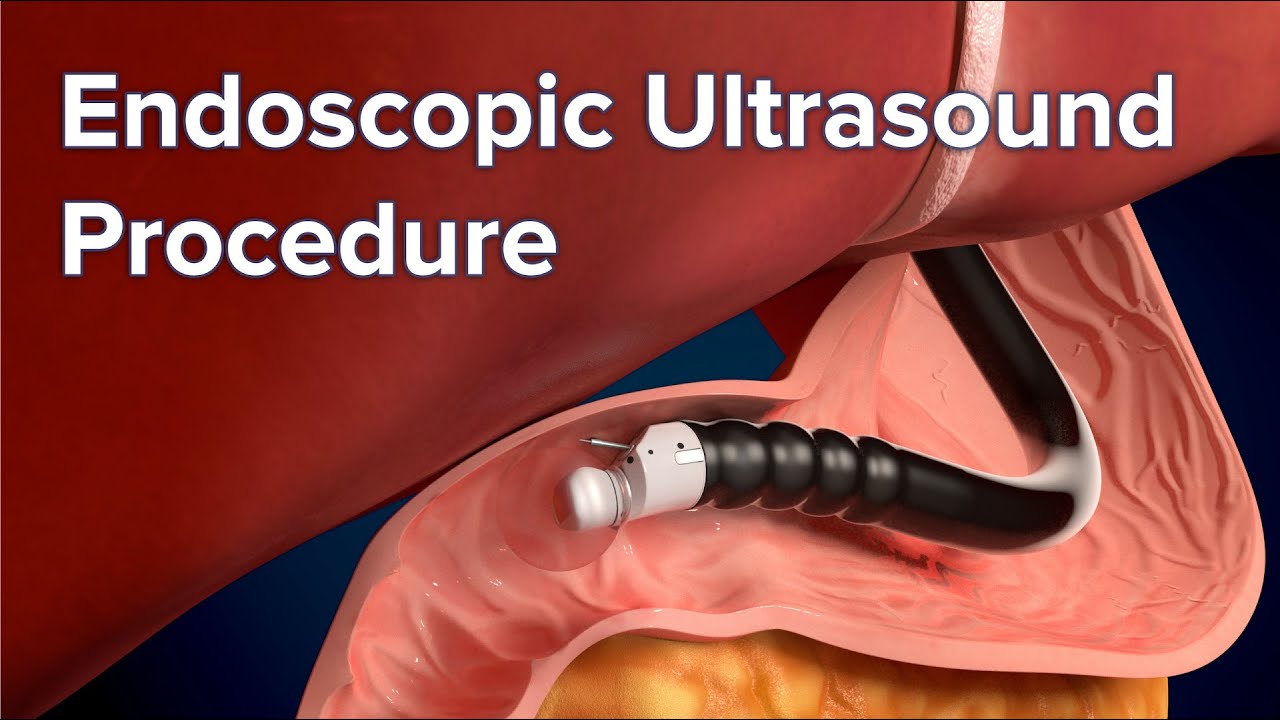
For this test, the doctor puts a short, thin, flexible, lighted tube into your rectum. The doctor checks for polyps or cancer inside the rectum and lower third of the colon.
How often: Every 5 years, or every 10 years with a FIT every year.
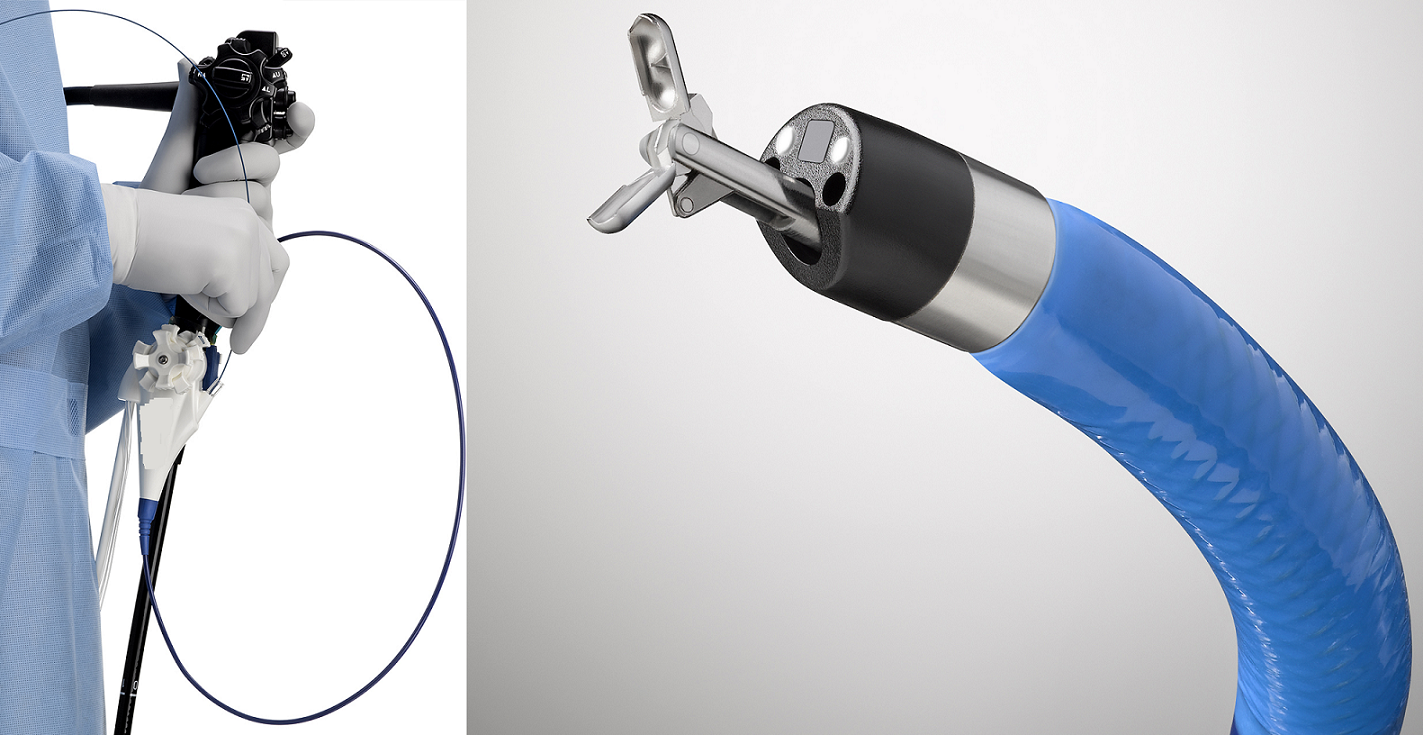
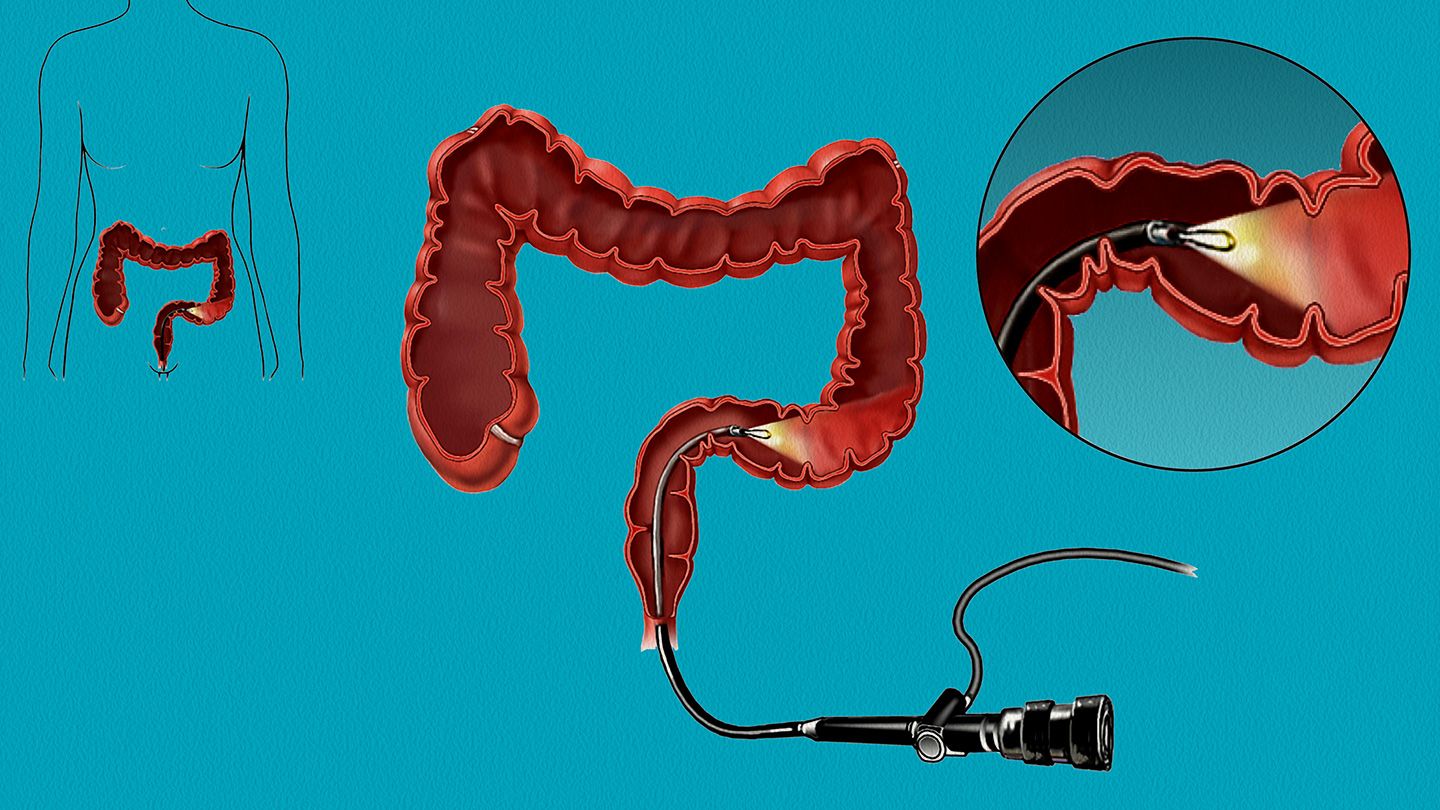
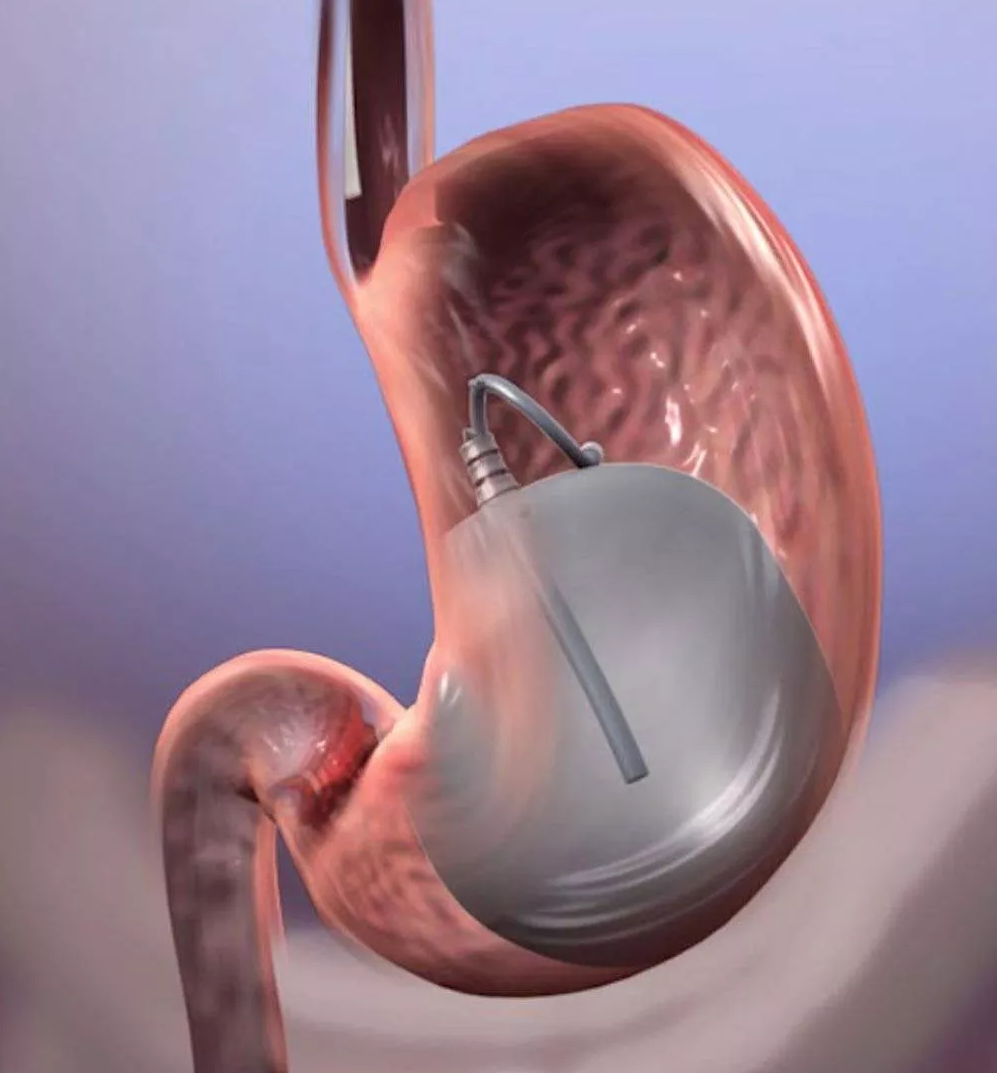
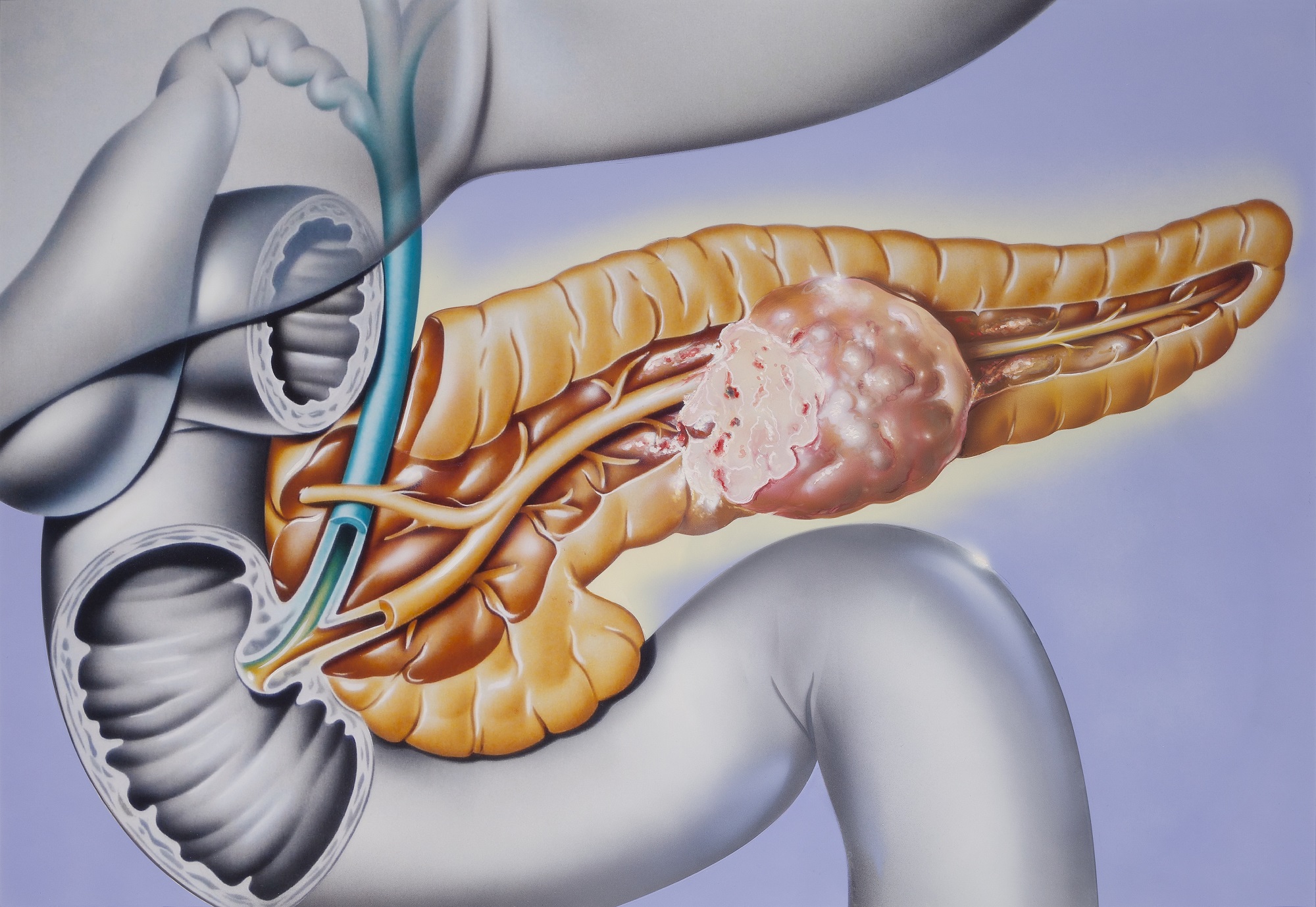
Colonoscopy
This is similar to flexible sigmoidoscopy, except the doctor uses a longer, thin, flexible, lighted tube to check for polyps or cancer inside the rectum and the entire colon. During the test, the doctor can find and remove most polyps and some cancers. Colonoscopy also is used as a follow-up test if anything unusual is found during one of the other screening tests.
How often: Every 10 years (for people who do not have an increased risk of colorectal cancer).
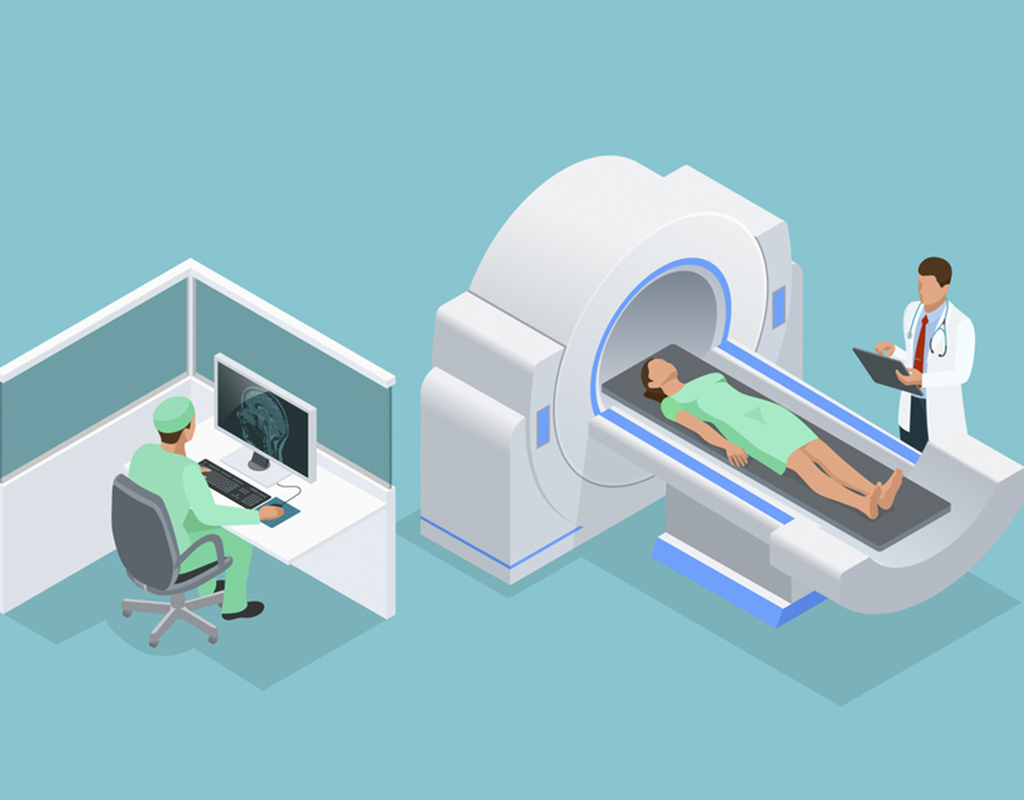
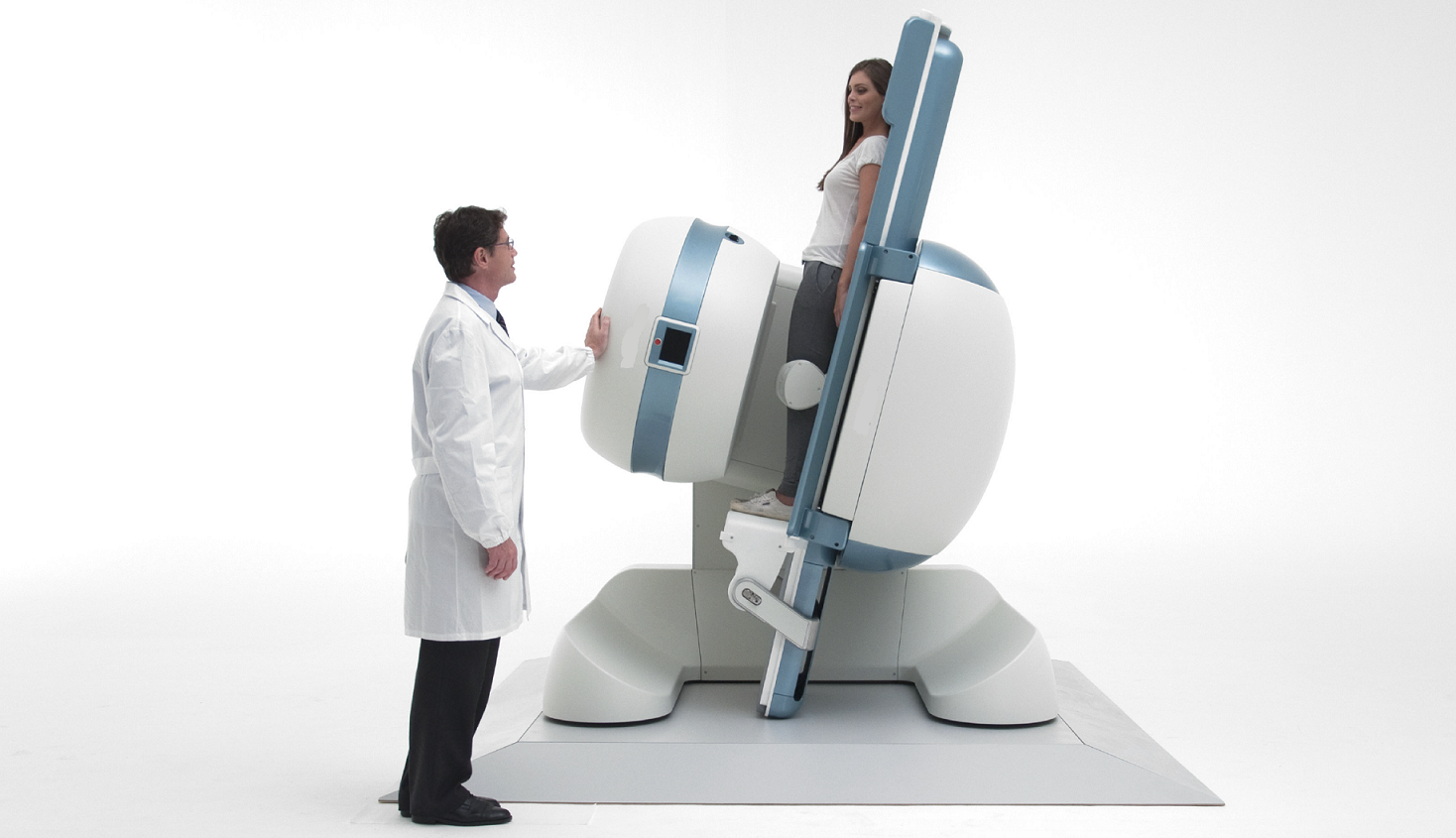
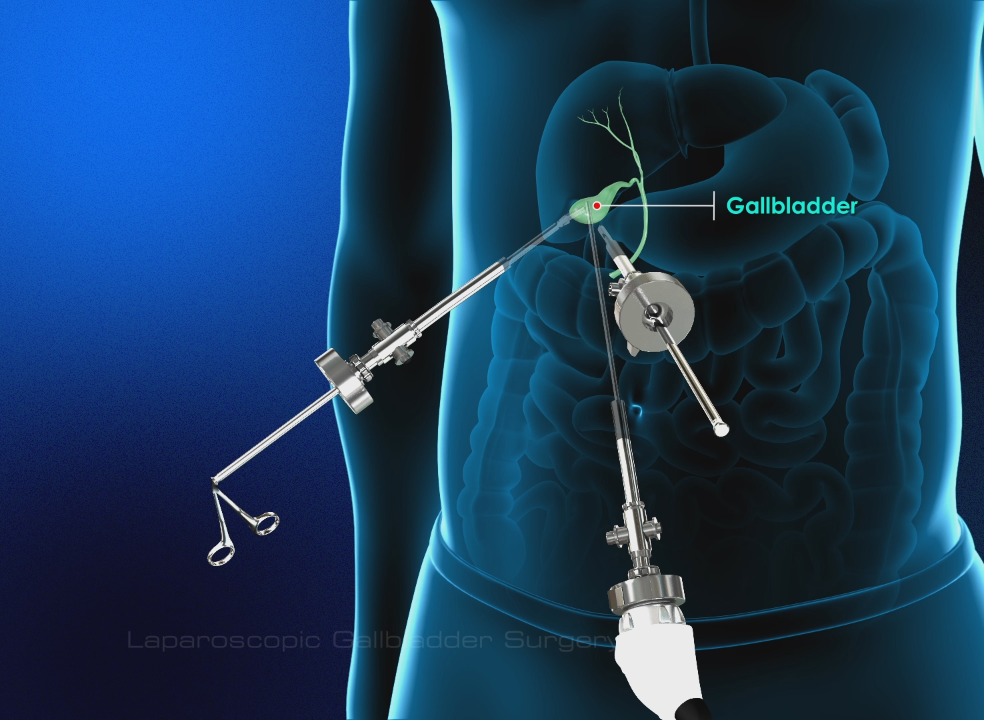
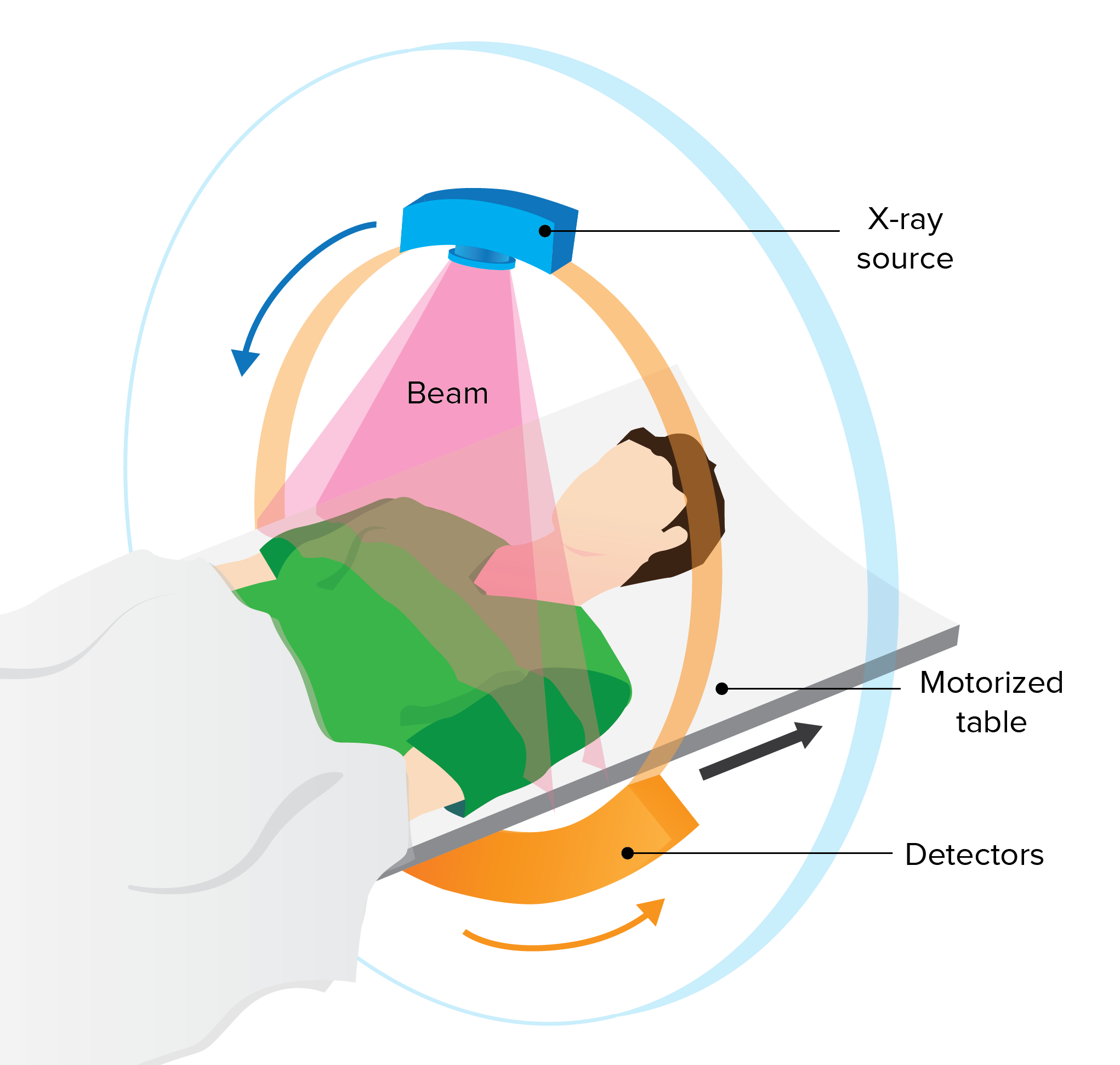
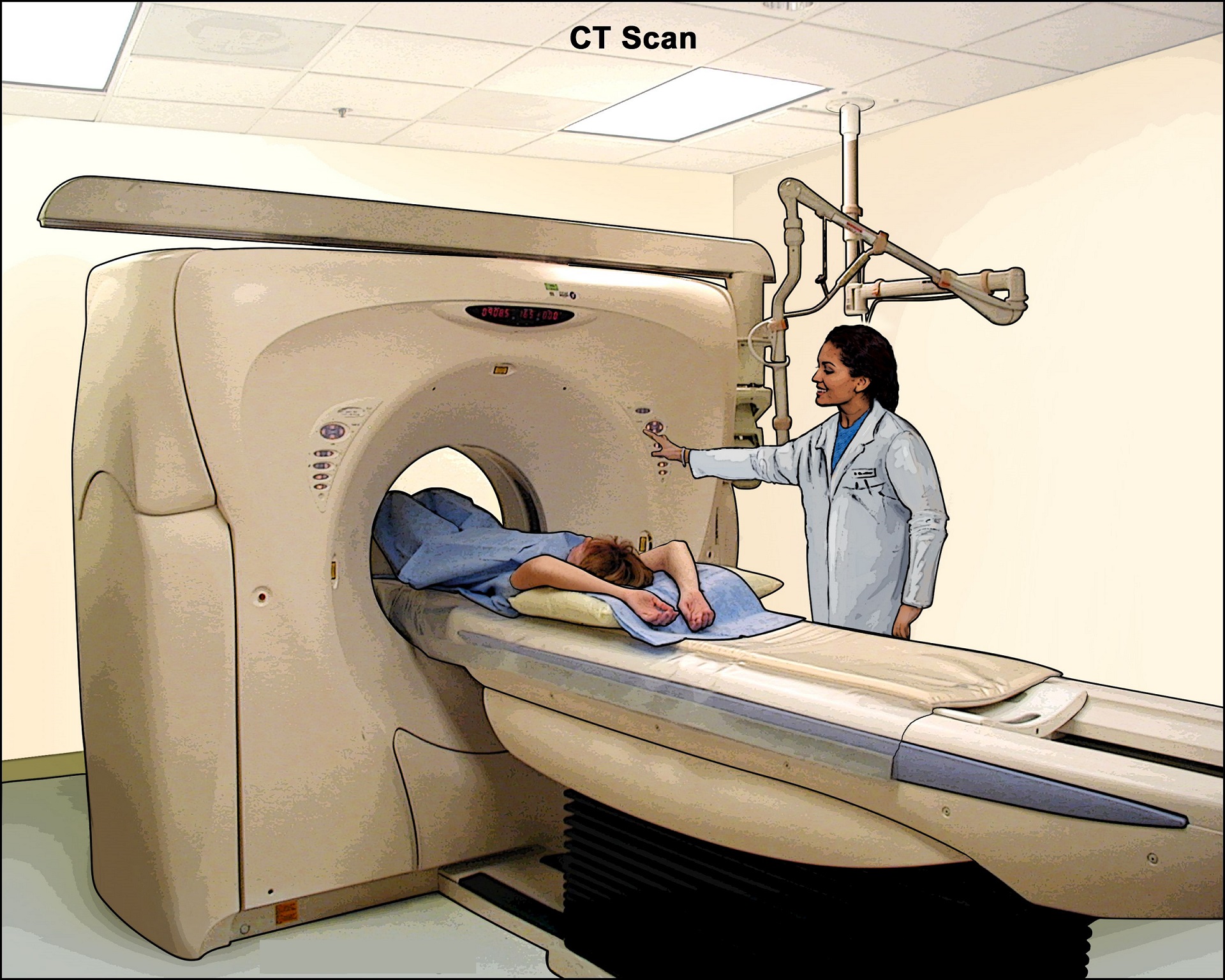
CT Colonography (Virtual Colonoscopy)
Computed tomography (CT) colonography, also called a virtual colonoscopy, uses X-rays and computers to produce images of the entire colon, which are displayed on a computer screen for the doctor to analyze.
How often: Every 5 years.
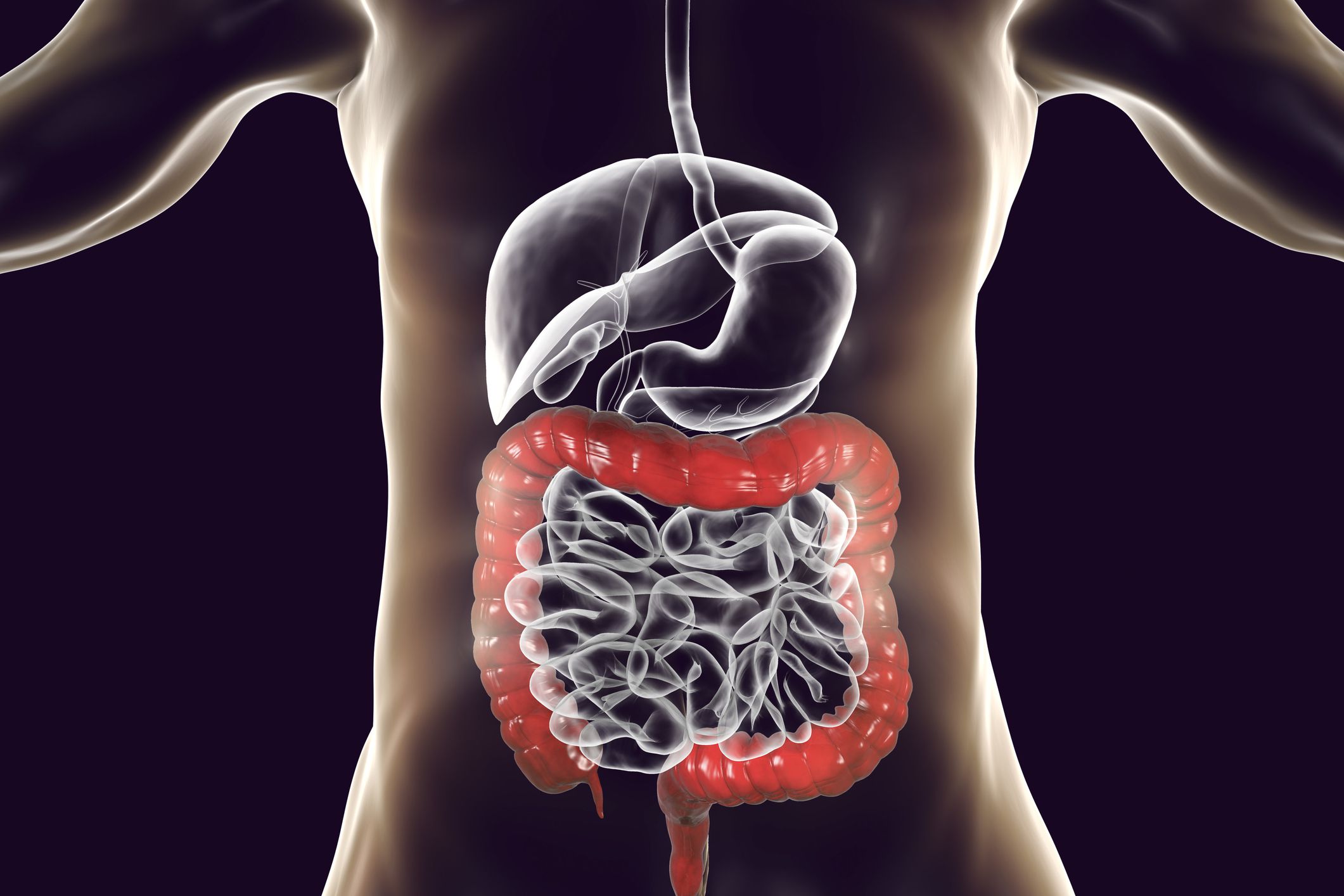
Diet
Research shows that diets rich in fruits, vegetables and whole grains are associated with a lower risk of colon or rectal cancer. Try to eat only small amounts of beef, pork and lamb, and eat fewer processed meats, like hot dogs. Eat whole grains, such as oatmeal, brown rice, popcorn and whole-wheat bread. Adequate vitamin D intake is also important. A large international study found that people with low levels of vitamin D had a higher risk of getting colorectal cancer.
Get active
Exercise could reduce the risk of colorectal cancer because it may reduce inflammation in the body and boost the immune system.
Watch your weight
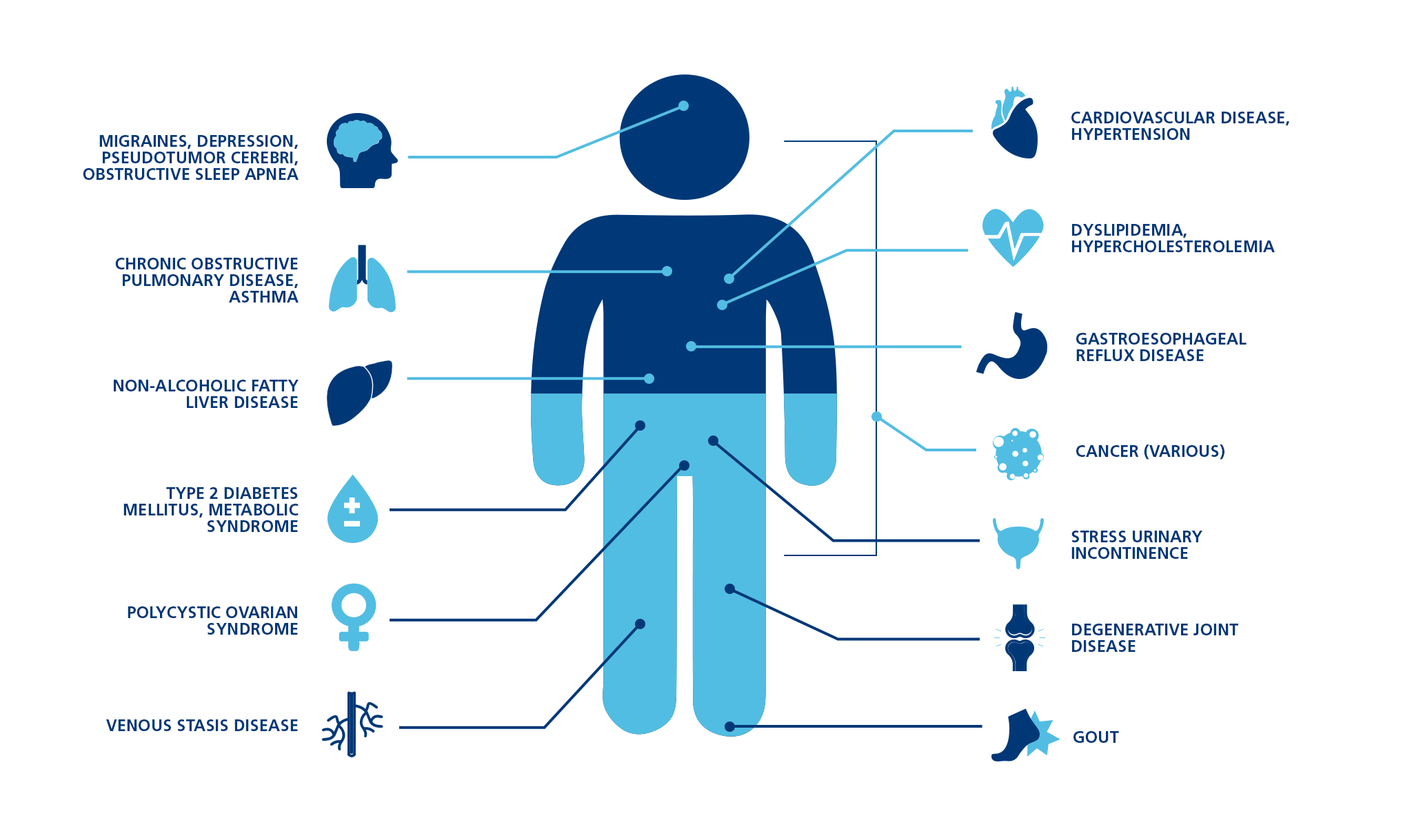
Being overweight or obese increases the risk of colorectal cancer.
Avoid or limit alcohol
Alcohol can cause intestinal damage. It is a toxin whose byproduct can damage DNA. The gut may develop inflammation, and the gut immunity is weakened. This can lead to colorectal cancer development. Limit alcohol consumption to no more than one drink per day.
Don't smoke
Several studies suggest that smokers have a higher risk of colorectal cancer than non-smokers or people who had left smoking a few decades back.
Book an online consultation with us here.
Reference
- https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
- https://www.mayoclinic.org/tests-procedures/colonoscopy/about/pac-20393569
- https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2360085/
- https://ods.od.nih.gov/factsheets/VitaminD-Consumer/
- https://www.cancer.org/cancer/cancer-causes/diet-physical-activity/alcohol-use-and-cancer.html